Had quite a shock when I went back to my surgeon this week. He confirmed my diagnosis was severe endometriosis. I had though it was mild to moderate.
He had warned me of the need for more surgery which I hadn't been keen on. I had started to brace myself for this bowel op after the sigmoidoscopy and bowel surgeon consult but it sounds scary. I said I knew about the risk of stoma and resection, I expressed my biggest fear as being the op being successful but still being worse or in pain as I am much worse since my first op which even didn't involve big treatment. Sex is now impossible im suffering severe fatigue and I have started to have bowel issues. He said though that the surgery would be more risky than expected because my bowel is actually distorted and tethered to my cervix. To date he has a clean sheet on stomas. He gave me another choice of zoladex injections plus tibilene to try to reduce pain and inflammation but that if successful that would then need to be followed by ovary removal oopherectomy. On asking his recommendation he said try the zoladex which surprised me.
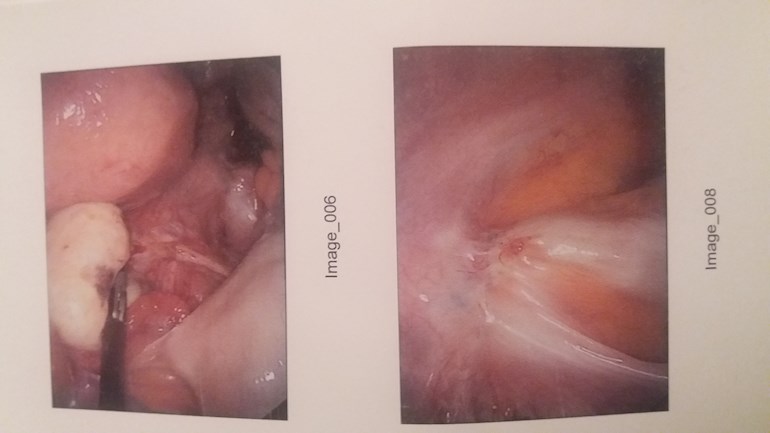
Having found on a quick search risks of oopherectomy so far I know it's a rare endo treatment when all else fails and risks are shortened lifespan dementia heart failure and cancer on ovary removal so I am wondering if the risk of bowel resection and Tumor removal may not be the better bet !! Here is one of the photos of Dave my nodule and the tetherimg to the cervix.
Had anyone else been in this dilemma and what did you do?