I have just received the results from my Blue Horizon thyroid +11 test today. Blood test was taken first thing in the morning, finger prick method, fasting. I have not been diagnosed yet with a thyroid disorder, but am pretty sure that's the case as my mother has and grandmother had thyroid disease.
Can anyone please give any suggestions in addition to the following doctor's comments? I have an appointment next Wednesday with my gp to discuss these results. Also, if anyone can recommend a good Endo in the Merseyside area, can you please pm me? Thanks in advance...
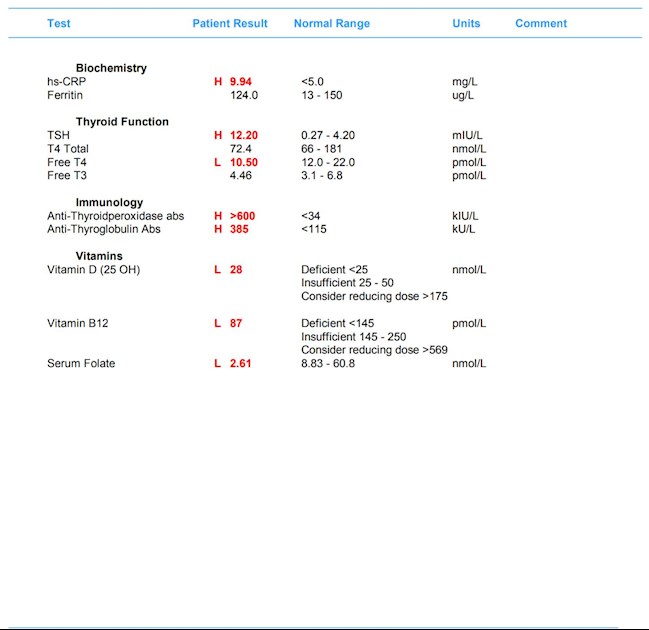
Results of test:
Doctor’s Comments
The Thyroid Stimulating Hormone (TSH) is elevated and the free T4 level is low . If you are already taking a form of thyroxine, it is possible that that your dose is too low or that you have forgotten to take it on occasion. It may be that an increase in dose is in order – if adjusted it would be sensible to repeat thyroid function (TFT) testing in around 2 months’ time. A normal free T3 level (in this scenario) could be a sign that you are taking liothyronine instead of levothyroxine. Is this the case? If so, it looks as though you will need upwards dose adjustment. However, if you are not taking thyroxine already, this result is likely to represent a new diagnosis of hypothyroidism (underactive thyroid gland). I advise you to discuss this result with your usual doctor as treatment, or adjustment is indicated. The positive thyroid antibody result, however, increases the possibility of your having or ultimately developing autoimmune thyroid disease, such as Hashimoto's thyroiditis or Grave's disease.
The High Sensitivity CRP level is elevated. Although an elevated level of this protein can be linked to increased risk of heart disease, more generally a high CRP (C reactive protein) is associated with inflammation (as seen for example with arthritis or infection) from some cause. It is not an exact test, and is non specific. Although the rise in your case is marginal, an elevated CRP is not a normal finding and its presence should lead to further investigation to establish the cause. It would be sensible to repeat this test around 4-6 weeks following this test as it may just be a temporary rise, but if persistently elevated it would be sensible to discuss this finding with your doctor.
The vitamin B12 level is very low. Some experts believe levels of 400-500 are desirable and that levels below this may lead to symptoms. Low Vitamin B12 levels can lead to Pernicious Anaemia (PA), a state of deficiency of the red blood cells in which there is reduced quality and number. Characteristically, the red blood cells are enlarged in this state (if the deficiency is severe and longstanding). A Full Blood Count is needed to check for this state, which is known as megaloblastic anaemia. Vitamin B12 is commonly found in many foods, particularly meats. Deficiency can develop if intake of the vitamin is reduced or if absorption from the gut is impaired. Poor absorption owing to a deficiency of Intrinsic Factor (IF) is the underlying reason for PA. Vitamin B12 deficiency in the longer run can lead to nervous system disorders - with sensation changes, loss of power or co-ordination, gut disorders and (rarely) dementia or mental illness. Lower level deficiency has been associated with a range of symptoms such as fatigue, memory impairment, irritability, depression and personality changes. Please discuss this finding with your usual doctor, supplementation and possibly further investigation is advisable.
There is significant Vitamin D insufficiency. Vitamin D is manufactured in our skin as a direct result of sunlight exposure. One potential complication of prolonged Vitamin D lack is osteomalacia, a disease which causes severe structural deformities to the skeleton. Lower level Vitamin D deficiency can lead to a number of non-specific symptoms, including possibly chronic fatigue (experts have for many years noted an association between sufferers of chronic fatigue syndrome or myalgic encephalitis (CFS or ME) and low blood levels of Vitamin D). It has been estimated that between 50-70% of people living in the northern Europe (where daylight length reduces your chances of receiving adequate sunlight in the winter) are deficient in this vitamin by March each year. Symptoms of vitamin D deficiency include chronic pain, weak bones, frequent infections (recent research has detected an association between vitamin D deficiency and severe pneumonia), depression and fatigue. Supplementation may be beneficial, I suggest you discuss this finding with your usual doctor.
The folate (folic acid) level is low. Folate is one of the B group of vitamins found in green vegetables in particular. The body's reserves of folate, unlike vitamin B12, are low and only sufficient for about four months. Causes of deficiency include reduced intake from the diet or from poor absorption through the gut; increased demand for folate (eg pregnancy) and side effects of some medication (eg methotrexate). Symptoms include fatigue, mild sensation changes and depression. Prolonged lack of folate results in megaloblastic anaemia (in which the red blood cells are characteristically large). Supplementation would be advisable - I advise you to discuss this result with your usual doctor.