It’s been around eleven months since my last post, so I thought I’d put together an update for those of you who are interested. It’s quite a long one. Apologies for that, but hopefully it will be of interest. It’s also helped me just to set it all out. A kind of therapy, if you will.
So, after a few delays for reasons I won’t bore you with, I eventually had the second operation on my spine in early December 2018. The surgeon decided to work only on T7, rather than T7 and T6, as he was concerned about the risks of paralysis etc. Mrs HighCadence was very pleased about that, and I guess I was as well, even though I’d initially been pushing for both vertebra to be removed to try get all the cancer in one go.
I’m not usually worried about operations, but this time I’d left strict instructions on what to do if I ended up paralysed; checked my surgeon’s hands for any sign of shaking before signing the consent form; and told the anaesthetist to give me a massive dose of morphine if anything went wrong during the operation. Funnily enough, that didn’t go down very well!
After the operation, the first thing I did when I emerged from the fog of the anaesthetic was to check for neurological damage by wiggling toes etc. When I realised that I was okay on that front, I checked the denervated area on my abdomen from the previous procedure to see if that had got any worse. That also appeared to be okay - so I was relieved, massively relieved.
There was some slightly bad news in the sense that one of my blood vessels had been cut during the operation - which meant that I had to lie flat for two days while the glue and collagen that was used to fix it set. That doesn’t sound particularly testing, but being completely flat for two days is quite hard. Try eating and drinking without sitting up. Straws become an essential part of life. Having said that, it was, of course, a relatively small price to pay for everything else being okay.
After that, I spent around two weeks in the hospital where one day blended into the next through the fog of OxyContin and a range of similar drugs. There were, of course, a number of challenges over that period. I was rushed off for x-rays and a CT scan when I couldn’t stop sleeping and my blood pressure and oxygen uptake were low (cue overnight magnesium and potassium drips); there was a scare over numbness that emerged in my right leg (cue more scans and tests before it was decided that it was simply the result of a nerve being trapped whilst I was in theatre rather than any damage to the spinal chord); and huge pain at the site of previous rib removal - largely linked to swelling caused by an inability to go to the toilet (thank you opioids).
I also had quite a few hallucinations. I won’t bother you with all the details, but my favourites were the time when I was standing trying to pee and the toilet suddenly turned into a glass fronted elevator on the outside of a building which then dropped around 20 floors; the time when my feet touched the bottom of the bed and the bed suddenly turned into a giant skateboard that I was riding around a skatepark; the time when my foot stated talking to me; and the numerous times when shadow animals moved around my room. All very interesting/exciting.
Through all of this, my wonderful wife and daughters visited constantly, and kept my spirits up - all whilst dealing with the impact of having builders in our house (we were extending our property), and preparing for a Christmas with visitors.
I have to admit that I’m often so wrapped up in my struggle with PCa and the side effects of treatment etc. that I forget my family is suffering too. They are on the journey/riding the rollercoaster with me, suffering the highs and lows associated with each visit to the oncologist, or news that emerges from scans and operations - to say nothing of the fact that I’m a difficult patient at the best of times.
We were helped this time by the fact that my room at the Wellington Hospital was much nicer than the one I had in the Brompton for the first operation. That meant everyone could visit and hang out at the same time if they wanted to. Indeed, there were a number of days when the whole family was together at the hospital eating and relaxing as if we were at home. My daughters also made sure to include me in the gift buying process ahead of Christmas, which, again, made things nicer/easier. Little things like this can make so much difference to how you feel when you’re lying in a hospital bed.
On release from the hospital I went home and was treated to a wonderful Xmas - managing to sit at the table for all of Xmas lunch before having to go back to bed with the OxyContin. Thoughtful changes had been made all around the house. I had a grabber to pick things up from the floor as I wasn’t allowed to bend down for three months. I also had a frame-chair-thing to help me get on and off the toilet, a chair to sit on in the shower, and a hospital table/tray in my bedroom. All good, although it did make me feel like I was 84 rather than 54.
A couple of weeks later, I started to feel quite anxious. It could be that I just have that programmed into me - more likely it was the impact of coming off the hard drugs. Mrs HighCadence had been slowly weaning me off them as advised by the pain management doctor, and that was the right thing to do because the pain from the operation had been subsiding. But, it was also very hard to do. Sleep becomes much harder - probably linked, in part, to the increase in anxiety. I was also incredibly emotional - bursting into tears all the time; I experienced huge swings in temperature, and had pains in all my joints - like the pains you get when you have flu.
To be honest, I made matters worse by refusing any top-up OxyNorm because I wanted to get off all the opioids as quickly as possible. That essentially led to three days of hell in bed with me ultimately having to take some small amounts of top up Oxy over the next week or so. After that, though, I was both free of the opioids and up and about a lot more often. Happy days indeed ... until there was blood in my pee, and everyone got nervous about the cancer spreading to my bladder.
The GP said I had to see a urologist immediately for scans etc. and looked very worried. I wasn’t. I’d been there before - in fact, I’ve lost count of the number of cystoscopies I’ve had over the years for this sort of thing ... so, I somewhat serenely sailed through a number of procedures that showed everything was okay/the blood was from damage caused by the catheter that was inserted during the operation.
A few weeks later, I had my six-week follow up with the surgeon. He told me that he didn’t have to take out the whole vertebra - he simply cut out the tumour until the bone became rock hard/too hard to drill into. Apparently this was the effect of previous treatment and/or the body doing its best to protect/heal itself. I took that as being good news.
Somewhat foolishly, I was hoping to be given the go ahead to start physiotherapy, but was told in no uncertain terms that I wasn’t allowed to do anything until at least three months had passed. Apparently this is the minimum amount of time needed for the screws that had been inserted into my spine to fully set.
Around this time, I decided it was time to buy myself a short scale/smaller/lighter bass guitar so that I could get back to playing ASAP and not lose all that I’d learned before the operation. It was all very exciting when it arrived and my daughter took it out of the box (vintage red with a cream finger board if you’re interested). But, of course, I couldn’t play it for even a short amount of time. I had to wait a couple of months for that. The choice essentially became either to reduce the pain killers or to play a bit of bass. I chose to reduce the pain killers so that I could “get my brain back”. The bass sat there looking at me accusingly from the corner of the room :).
As I weaned myself off the opiates, I was slowly able to concentrate a bit more, so that reading something longer than a tweet or snippet of news became possible. I was also able to draw - something I hadn’t done for years. Dog walks became a focal point of my daily routine - with progress measured by how far I could get round the local park before I needed a pain killer. At first it was half a lap. Then a lap. Then not until I got home, and then, as if by magic, not at all.
Although this was encouraging, the fact of the matter was that I was bored, really bored. I’d been at home in some sort of recovery for almost three years by then. There wasn’t a TV box set I hadn’t watched, a book I hadn’t read, or a podcast I hadn’t listened to. I wanted to ride my bikes, go to the gym, and play my guitars. I wanted to be able to walk at my normal pace, sit comfortably in a chair (dear God, I’d have given my right arm for that), and to climb the stairs to the top of our house without almost collapsing through shortness of breath. I wanted to be free of drugs that affected my thinking, and the withdrawal effects when you try to come off them. Goodness me, I know we have to have these drugs, and I’m really grateful that they are available, but I wonder how often they would be prescribed if the prescribers had to first experience the withdrawal effects when you try to get off them. Pregabalin, is my biggest bugbear on this front. It’s great for nerve pain, but when you try to reduce the amount you take, you get incredibly anxious, it’s almost impossible to sleep, and you end up feeling really low.
When I got to that point, I decided to get myself out of the doldrums by sorting out the next stage of treatment, which, in my mind, was always going to be PSMA targeting. I looked for links about this treatment on the forum, and, as if by magic, found myself on a thread which took me to a post, and then another post which mentioned both the Vision trial and the fact that the London Clinic was offering the treatment. I’d assumed I would have to go to Germany for this, but now there were two options which would mean I could stay in London for the treatment. Wow, I was really excited by that. But, hold on, why hadn’t my oncologists told me about this? You know, the ones I’d told that I wanted to have the PSMA treatment ASAP? Hmmm, not good. Indeed, I was reminded of the old adage that the person that cares most about your health is always you, and that the harder you look, and more determined you are to find solutions, the more likely you are to find them. I came late to the forum, but, without it, I would have taken a lot longer to find out about a treatment I think holds promise for a large number of us - perhaps having first gone down less promising/unnecessary routes. I try to remind myself of this when I’m looking at my emails and telling myself that I just can’t face any cancer stuff today.
So anyway, I followed up with the London Clinic, and the Vision trial team at Guys. This proved to be a bit long winded. The London Clinic hadn’t really started the treatment, and I got sent to the wrong clinic at Guys, who were also only just getting started. I also had to approach the insurance company to see if they would fund the treatment if I didn’t get a slot on the Vision trial.
In the meantime, my first PSA test after the operation. came in at 7 - exactly the same as before the operation - so the remaining hotspots were obviously getting a bit more active. I was a bit worried about that, but then got a call from The Royal Marsden during which I was told that analysis of the tumour that was removed from my spine showed I had micro-satellite-instability (MSI). Apparently, this is a good thing, in the sense that it means immunotherapy/targeted immunotherapy is more likely to work. So that’s a possible route to go down in the future - although my BRAC2 mutation was supposed to make Olaparib work, and it didn’t. I was also told that latest/unpublished research shows patients with the BRAC2 mutation do better with PSMA targeting - because their cancers tend to express more PSMA. Overall then, these genetic faults of mine were actually positive news - well, that’s how I was viewing them.
So, I told myself again that I simply had to get onto the Vision trial. That proved to be a little tricky. First, I was told the fact that I’d had radium 223 within the last six months ruled me out of the trial ... damn it. Then I was told there was a 20% chance they might let me on anyway ... great! Then finally, that I was on the trial ... fantastic ... but then there was a bit of a dance around whether or not my insurance company/I could pay for the treatment instead, and whether or not I’d stay on the trial if I was randomised to have best standard of care rather than the lutetium. I’ve got lots of views on how this stage was handled, but they are not for this forum. Maybe I’ll divulge more in the future.
Anyway, after a bit of toing and froing, I eventually had a CT and PSMA scan to determine if I was right for the Vision trial i.e., whether or not I was PSMA avid. I was, so then went through to the randomisation stage. We all held our breath, the computer button was pressed and ... and ... and ... and .... I DIDN'T get the lutetium arm of the trial. Damn, damn, damn, f@ck, f@ck, f@ck. Two months had passed and I was no closer to getting the treatment I was convinced was the best next step. Worse still, I was informed that best standard of care was deemed to be no treatment at all. WHAT? How could that be right? I didn't want to have some more chemo or go on an immunotherapy trial at that stage, but shouldn’t these be seen as best standard of care? Given that, it took me only a few minutes to decide that I would not be staying on the Vision trial. I would, instead, pay for the lutetium treatment myself.
Fortunately, the insurance company agreed to pay for some of the first few rounds of treatment, which was clearly a help. But, they would only do this via an an off-policy contribution that would be treated as a taxable benefit to me, so I would effectively have to pay half of the cost of the first few treatments and for all of the cost of any further cycles. Oh well, I decided I’d just have to use the “rainy day account”. I couldn’t sit back, do nothing, and watch a really good treatment option disappear over the horizon.
I felt bad about having to use our savings to do this, as my priority has always been to leave as much as possible for the family when my treatment options run out, and I go off to find out what happens after death. But, it had to be done. I also felt bad about dropping out of the Vision trial, as they needed people to stay on the best standard of care arm. But, my PSA had by then risen to 11.5 and was increasing fairly quickly. I had to put myself and family first. I’m 54, with a wife and two children still at home. So, it was game on at the London Clinic.
Except ... it wasn’t. Getting my scans sent over from Guys Hospital proved to be extremely difficult - so my case wasn’t discussed at the next weekly multi-disciplinary team meeting. The following week, I was assessed/approved, but the lutetium wasn’t delivered (something about a temperature gauge being damaged in transit). I was then told I had to have a kidney scan - a proper step, but a step that could, and should, have been taken earlier. Days had turned into weeks, and weeks into months. I was starting to panic.
However, a few days later, when I was just about to get my haircut, I got a call from the London Clinic suggesting I switch to Genesis Care in Windsor as they were already up and running with the treatment, and the London Clinic really didn’t know when it would get the lutetium. Probably mid-June, but it couldn’t really say for definite. Indeed, it had been expecting to be up and running since the previous November. So, the following Monday, my wife and I headed over to Windsor and met Dr Yong Du (who gave me radium 223 at the Marsden). Very quickly it was agreed that I could start treatment on the following Thursday.
From other posts on the forum, I’ve seen that people are very interested in the ”mechanics” of lutetium treatment, so this is what happened to me for the first cycle:
Picked up at 09.00 (this service is part of the package and is needed for reasons I’ll outline later).
Arrive in Windsor at 10.30.
After filling in some induction forms, I was then taken through to a small windowless room at 11.00. There isn’t enough room for another person to be in there with you - which is good, because they aren’t allowed anyway.
Everything is covered with clear sticky back plastic in case there is any spillage of the lutetium. I assume this is removed between patients.
You are given a bag with a water bottle, some reading material and information on the treatment.
A cannula is put into your arm and you are hooked up to a saline drip.
You are then asked to complete some questionnaires on how you feel, what your pain levels are, what’s going on with sexual function etc.
Three vials of lutetium were then inserted via the cannula at around 11.30.
I then went back on the saline drip for around another hour or so.
After the drug had been put into me, there were half hourly checks on the radiation that was being emitted from me. The doctor literally held a one metre ruler out from his chest to ensure that he didn’t ever get too close to me.
Lunch arrived at around 12.30 (you chose from a good menu).
Once the saline drip had run through, and they were happy with the radiation levels, I was allowed to go home.
For the first week after the treatment I was not allowed to get within a metre of anyone else for more than 15 minutes. This meant sitting on the back seat of the car on the opposite side to the driver on the way home (thus the car service), and sleeping alone. I more or less stayed away from family and friends for the first week after the treatment, but you probably don’t have to be so strict. I felt like a bit of an exile in my bedroom when I probably didn’t really need to.
For week two, the restrictions only applied to being close to small children and women who could potentially be pregnant. I asked about our little dog, but was told that that didn’t matter as dogs don’t live long enough for the radiation to be an issue!
On the day of the treatment I was fine. There were no problems during the injection/infusion. My mouth started to feel dry and my saliva glands a little bit sore around 6 hours later. But this was marginal, rather than significant. My wife and forum posts reminded me to drink a lot, and that helped. Overall, I’m not sure I would even have noticed the effects if I hadn’t been looking out for them.
On the day after the treatment everything felt like a bit of an effort - especially when it came to walking up stairs (my nemesis). There was a bit more pain in my spine than usual, but I was still quite active, doing some work in the garden, and practicing my bass guitar etc. It was all just a little bit harder to do.
That feeling got worse on day three. Indeed, I was tired to the pit of my stomach, so had to rest up a bit more.
The following day, I dozed off after a morning of working from home - something I can never usually do. And when I was awake, I was a lot clumsier than usual. On the plus side, there was no longer any pain in my spine. NO PAIN IN THE SPINE FOR THE FIRST TIME SINCE THE OPERATION, which was great, right? Ah, well, hold on. I’d read a lot about pain and lutetium treatment on the forum, and that suggested increased pain was good - a sign that the treatment was working/messing with the cells in the mets. So, no pain was bad ... unless it was simply a sign that my physical recovery from the operation had taken a step-change for the better ... which would be good, but in a different way, right? And so, this cycle of thought went round and round in my head for hour after hour. No pain was good, no bad, no good ... repeat to fade. Eventually, I decided that I’d just have to wait for PSA and scan results before I’d know the truth.
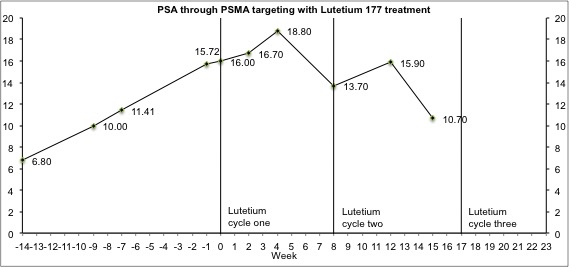
And so, the “tyranny of the blood test” took centre stage once more. At the start of treatment, my PSA had risen to 16. Two weeks after the treatment it had ... RISEN ... to 16.7 .... sh@t, sh@t, sh@t. But hold on, I knew from the forum that this test is meaningless/that an increase in PSA at this point could be a sign of the treatment working, so I took a deep breath and waited for the test at week 4 ... and ... IT WAS UP AGAIN (at 18.8). Worse still, the oncologist was avoiding eye contact with me when he told me the result! ... f@ck, f@ck, f@ck. it’s not working, it’s not working, it’s not working, it’s not working. The terror took hold. I was panicky, and not sure what to do next. The oncologist said all the right things i.e. the treatment is new, they didn't really know what pattern PSA usually follows, and this could be a sign the treatment is killing lots of cancer cells - so stick with it, have the second cycle and see what the scans show up after that. Dr Yong Du said the same, and told me that roughly 50% of patients see a decline in PSA after an initial spike. I knew this was the sensible approach, but have to admit to being very disappointed/worried. I’d read all the reports on the treatment and it seemed to me that there was either no response or a very significant response to the lutetium. So, I went ahead trying to be optimistic, but secretly fearing the worst.
The second cycle followed the same procedure as the first, except the lutetium was now in one container rather than three. In the days after the infusion I felt a bit “blah” again, experienced an increase in pain in my spine and had a bit of a temperature rise - although the latter could have been related to an infection at the site of my latest zolodex injection that had been building up over a few months. The pain in my spine could also have reflected the fact that was doing more - especially in the garden, and at the gym. so God knows what I was supposed to make of it all.
All this made me very antsy/anxious and, because of that, fairly short with friends and relatives. So, it was with a large amount of trepidation that I contacted Windsor to find out the results of the blood test I’d had on the day of cycle two. The email pinged into my inbox, I opened it and ... PSA DOWN, PSA DOWN!! (to 13.7). Wahoo! Dear God, this was turning into some rollercoaster ride.
A week or so later, feeling much more positive about the treatment, we flew out to Corsica for a much needed family holiday. Although there were lots of problems with our flight, I’m pleased to report that neither the radiation from the treatment, or the rods in my back from my operation caused problems with airport scanners etc.
And so we relaxed into our holiday. This time round, the treatment had more of an impact on my mouth. Indeed, after about 10 days, it felt like my tongue was burned and I had the ash-like taste thing you get from chemo. But, that only lasted for a few days. Sucking sweets and drinking helped limit the impact while it was there.
So, everything settled down, and we got into the swing of relaxing in the sun, reading books, swimming etc. But as I’m sure you are now aware, nothing runs smoothly for me for any length of time. Indeed, whilst I was lying down on the sun bed reading about four days into the holiday, I suddenly noticed lots of black floaters and millions of tiny dots on the surface of my right eye.
I’d already had a lot of blurring in that eye that I’d put down to a side effect of the pregablin, and I’d also been given some new meds before we went away that could have been the cause of such a problem. But, to be sure, I checked with my GP. The response was equivocal, so, on my return from Corsica, I had another PSA test, then went straight to see my local optician. Long story short, my retina was detached, I had to go straight Moorfield’s eye hospital, and a day later I was lying on an operating table having my retina sewn back into place! The operation didn’t hurt, but afterwards I had to lay flat/on my right side for five days so that the gas bubble that had been inserted into my eye held everything in the right place. And when I say five days, I mean five days solid. You are literally only allowed to sit up for ten minutes of every hour.
To make matters worse, I’d missed my appointment with the oncologist, so I had to send the “can I please have my blood test results?” email. The response came back fairly quickly, I pressed the open button, and ... and ... PSA IS UP AGAIN (to 15.9). F*ck, f*ck, f*ck, f*ck, f*ck!!! Give me a break! Just one break! But, of course, cancer doesn’t work like that, does it? I just had to tell myself that this is exactly what had happened at the same stage of the first cycle and pray for a lower number next time round.
To be honest, I was feeling a bit low at this stage. My eye was sore, my PSA disappointing, the wound from my hormone injection still hadn't healed after lots of antibiotics, and I was getting more short of breath by the day. So, I trudged off to my PSMA scan and latest blood test fully expecting to be hit by lightening on the way (If you ever meet me in person I’d advise not to stand too close as disaster is always just around the corner!).
The scan was a bit difficult because it’s a problem for me to lie down on a hard surface due to the screws etc. in my back. But, it only took 25 minutes, so was finished just when I was at the point of telling the technicians that I couldn’t really go on for much longer. I was, at that point, also feeling really tired. In my heart of hearts I knew that was probably because I’d gone back to work again after the operation on my eye and was increasing my hours. But, in my depressed state, I managed to convince myself that it was because the cancer was taking hold again. So, when Dr Yong Du called me to talk through the results the next day, I wasn’t really expecting anything positive. First off, he told me that my PSA had .... FALLEN (to 10.7). Yes, yes, yes! I know we’re not supposed to focus entirely on PSA, but it’s my go-to start-point when thinking about disease progression etc. He then told me that the met in my lymph node had shrunk a bit. Yes, yes, yes. Finally, he told me that all my other mets were at least stable. Well, that might not be the kind of results I’d hoped for at the start of the treatment, but I was happy to take them. We move on to cycle three at the end of this week/tomorrow.
So, what to make of all of this? First off, was the operation worth it? Well, it’s been really hard. I’ve outlined some of the problems above, but there’s also been an endless amount of physio to try to get back some level of fitness. I’ve had problems trying to reintegrate back into work after being out for five months I have a very supportive boss and team of colleagues, but it’s hard for them to judge how I’m feeling. They can see that i look a lot better than when I was in hospital, but they can’t see how mushed my brain has been at times because of the tablets I was taking. And then there is the fact that the nature of my work is very time specific. It needs to be completed quickly. But it’s very hard to get anything done in a timely manner when you’re only working one morning a week, or two, or three. So I’ve been very anxious about that. Just to be clear, there has been no pressure from my employer - they’ve been very good - the stress is largely self induced. But, I’ve suffered quite a bit because of that.
So, I guess what I’m saying is that if you are faced with the choice of an operation don’t go into it lightly. But, when you think about it, what else could I have done? Spinal chord compression was looming. I had to act. If it had been a year later then I would have gone down the PSMA targeting route. But you have to face the cards you are dealt and keep moving forward. It’s all you can do/what you have to do. Overall, I’m pleased I did it.
As for the PSMA targeting treatment, I’d be lying if I said that results were as positive as I’d hoped. But, they have been positive. The PSA path is a bit unnerving (to say the least). But it seems with me that PSA initially goes up for the first four weeks of the cycle, then slowly comes down over the next few weeks. If my bloods hold up - I’m as anaemic as I’ve been for years at the moment - then a few more cycles could push my PSA down to a much lower level. Apart from the anaemia, the side effects of the treatment have been minimal for me, so I would fully recommend it.
Well, that’s about it. Apologies for such a long-winded post. Hopefully it will be useful to at least some of you. I’ll let you know how the next cycles of Lu-177 go. Take care, and good luck to you all.
 Hope your health is good.
Hope your health is good.