I am new here and would be grateful for any input.
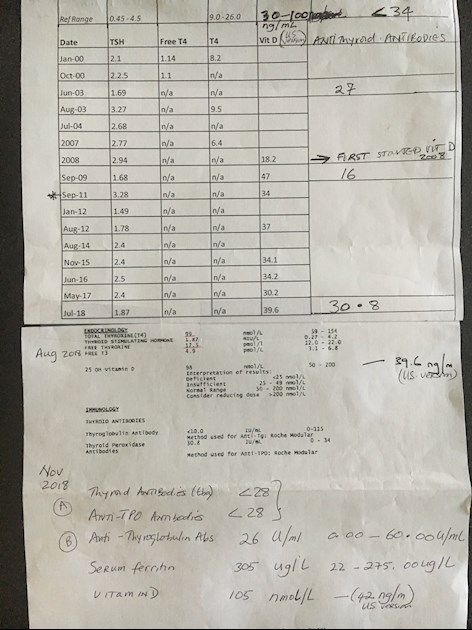
I have Hashimoto's and have been on medication for about 15 years, currently taking a combination of T4 50mcg and T3 2.5 mcg, which I do well with. I have a strong family history, my maternal aunt had and my sister have Hashimoto's. For the longest time I have believed, from observation of symptoms, since childhood, that my adult son has Hashi's although blood tests reveal levels in the normal range with no presence of antibodies.
My son's symptoms include: cognitive problems, memory loss, depression, apathy, very high ferritin levels( haemochromotosis test negative) muscle and joint aches and pains, edema, hair loss, high cholesterol, metabolic syndrome, weight gain (despite a good diet) sleepiness, IBS, fatty liver, chronic fatigue, inability to tolerate exercise, and inability to tolerate any supplements except vitamin D. Many symptoms have progressively worsened.
Last year he had an Ultrasound that showed a "rough textured thyroid" which was otherwise normal. A London endocrinologist said his thyroid was "large" but tests and a scan showed normal results. An endocrinologist in the U.S on seeing the images said he has non serum positive Hashimoto's thyroiditis. That antibodies are present but there isn't an assay smart enough to detect them yet. He advised a TSH test every 3 months, no medication until the thyroid has stopped swinging to and fro and the TSH is around 5 and anti depressant when needed. Meanwhile the symptoms continue and we control as much as we can through diet and lifestyle, this does not appear to be enough.
In November his B12 levels were 361( reference range 187-883) and serum folate was 6.4 ( reference range 3.10-20.50). We are both heterozygous for the MTHFR gene.
Because of the autoimmune component it is crucial to get an accurate diagnosis so I did an ultrasound of my thyroid. The radiologist said if I had not told her I had Hashi's she would not have known and that my thyroid was" normal". She compared my images to that of my sons concluding both thyroids looked the same. The difference is I have antibodies. But our symptoms are very similar, particularly compared to the period before I was on medication
My questions:
1. Would a trial of medication be damaging and have adverse effects i.e. if he did not do well and had to stop, would the symptoms worsen. Would he be likely to develop nodules? How long can one go on a trial, bearing in mind we are all so different in our responses.
2. What would be the common side effects to look for on medication? I would try him on a combination as I am of T3 and T4.
I am aware Synthroid depletes the body of iron, B2 and calcium and increases the risk of osteoporosis.
3. Is it better to start medication if this is the early stages of Hashi's or wait . I have read that if there are antibodies even low numbers, treatment must start immediately, but this is not so in my sons case, but the symptoms are very prevalent. But is it better to focus solely on the autoimmune aspect ? we do focus heavily on gut health.
4. Are there any sources I can go to to find an endocrinologist that will accept there is a need for medication despite "normal" labs? we are currently in the London area but I will go anywhere to find the right person.
Thank you for taking the time to read this.