Fibromyalgia: An Afferent Processing Disorder Leading to a Complex Pain Generalized Syndrome (2011) Howard S. Smith, MD1, Richard Harris, PhD2,and Daniel Clauw, MD2
A few comments will be seen in bold
This study mentions the overlap among fibromyalgia, CFS, and avariety of regional pain syndromes as well as psychiatric disorders – and shows that the common underlying pathophysiological mechanism seen in most individuals with fibromyalgia, and large subsets of individuals with
these other syndromes, is central nervous system (CNS) pain or sensory amplification.
The current thinking about these overlapping symptoms and syndromes is as follows:
• Groups of individuals with these conditions (e.g.fibromyalgia, irritable bowel syndrome [IBS], headaches,temporomandibular joint disorder [TMJD], etc.) display diffuse hyperalgesia (increased pain in
response to normally painful stimuli) and/or allodynia
Here in the community we often mention other associated illnesses including Plantar Faciitis, IC. Costohrondritis etc - interesting isn't it?
Although pain and fatigue are 2 of the most common fibromyalgia symptoms, sleep disturbances
and sexual dysfunction occur very frequently as wellin fibromyalgia patients.
I thought this may be of interest to meembers who have recently posted about personal issues
In addition to pain and sensory amplification, other shared mechanisms and/or epiphenomona include neurogenic inflammation,especially of mucosal surfaces, leading to increased mast cells and the appearance of a mild inflammatory process; dysfunction of the autonomic nervous system; hypothalamic pituitary dysfunction.
In addition to the heightened sensitivity to pressure noted in fibromyalgia, other types of stimuli applied
to the skin are also judged as more painful or noxious by these patients as well. Fibromyalgia patients
also display a decreased threshold to heat, cold, and electrical stimuli
A comment about how debilitating it can be compared to other conditions, interestingly, as many of us say how it effects our quality of life. As with the lack of Awareness & understanding many people may not realise this , however this as a statement may helpp help people to realise how debilitating it is as compared to RA, OA, COPD & IDDM he (conditions that people understand)
Fibromylagia affects all aspects of daily physical functioning. Women with fibromyalgia consistently
scored among the lowest in quality of life measures versus women with rheumatoid arthritis (RA), osteoarthritis (OA), chronic obstructive pulmonary disease (COPD), or insulin-dependent diabetes mellitus (IDDM). Patients with fibromyalgia have reported difficulty with multiple activities (41,42). Sixty-two percent have difficulty climbing stairs, 55% have difficulty walking 2 blocks, and 35% have difficulty with activities of daily life
Functional MRI studies (pictures in free text article)
Brain imaging studies also support the existence of central pain augmentation in fibromyalgia, IBS, low
back pain, and several other of these conditions . Gracely et al performed the first functional magnetic resonance imaging (fMRI) study of fibromyalgia patients in 2002. When stimuli of equivalent pressure magnitude were administered to fibromyalgia patients and controls, Gracely and colleagues found increased regional cerebral blood flow in fibromyalgia patients compared to control participants who did not have fibromyalgia
Interesting excerpt about neurotransmitters, susstances in CSF and also discussion again about the lack of efficacy of Opioids in Fibro
In fibromyalgia, there is evidence for increases in the CSF levels of substance P, glutamate, nerve
growth factor, and brain derived neurotrophic factor, and low levels of the metabolites of serotonin,
norepinephrine, and dopamine , any of which could lead to an “increase in the volume control”
and augmented pain and sensory processing The only neurotransmitter system that has been
studied to date and not found to be out of line in a direction that would cause augmented pain transmission is the endogenous opioid system. Both CSF levels and brain activity by functional neuroimaging appears to be augmented, not reduced (as would cause augmented pain processing) in fibromyalgia, which may be why opioidergic drugs do not appear to work well to treat fibromyalgia and related pain syndromes
Strangely, we have always mentioned this to members that what works for one may not work for another
It is of note that any one of these classes of drugs only works well in about a third of patients, which is
entirely consistent that this is a strongly genetic – but polygenic disorder – and thus different treatments are needed in different individuals
Please see the section about the Diagnosis and Assessment of Fibromyalgia in the full article if of any interest
Interesting a possible new treatment under research? Tizanidine - anyone taking this already?
A quote from the Pharmacological Treatment of Fibromyalgia Tizanidine is a centrally acting alpha-2 adrenergic agonist considered a muscle relaxant which might have beneficial effects on spasticity. Tizanidine might produce significant improvements in several parameters in fibromyalgia including sleep, pain, and measures of quality of life . Additionally, tizanidine treatmentresulted in a significant reduction in substance P levels in the CSF of patients with fibromyalgia.
Information about Tizanidne patient.co.uk/medicine/tiza...
Some information about Tramadol explaining the way it works to provide analgesic plus is Tapentadol a potential treatment to next be researched
Tramadol is a compound that has some weak analgesic effects by binding to the mu-opioid receptor, but the majority of its analgesic effects are from serotonin/norepinephrine reuptake inhibition. Tramadol appears to possess some beneficial effects in the management of fibromyalgia both alone and as a fixed-dose combination with acet-aminophen (153,156,157). Tapentadol, an atypical opioid
that has some opioid effects as well as inhibits the reuptake of norepinephrine, has not been studied yet
for the treatment of fibromyalgia
Information about Tapentadol patient.co.uk/medicine/tape...
We often talk about relaxation techniques and here PMR is discussed so have added it as many of you say it does help alongside other treatments
Relaxation techniques are commonly part of CBTfor fibromyalgia, (211,213). Relaxation techniques likely to be helpful for fibromyalgia symptoms include but are not limited to PMR, autogenic training, guided imagery,and meditation.PMR involves the systematic tightening and relaxing
of various muscle groups with the goal of decreasing muscle tension overall, and thus ameliorating anxiety, which was presumed to be linked to muscle tension. Patients with fibromyalgia should be cautioned not to tense their muscles too tightly during this exercise because this could result in exacerbating pain.
A conclusion excerpt and prognosis discussion
In the past decades, our understanding of fibromyalgiahas evolved tremendously, and the study of
fibromyalgia has taught us about the mechanismsthat might underlie chronic pain or other somatic
syndromes, in individuals without fibromyalgia per se. A better understanding of the underlying mechanisms and most effective treatment for this spectrum of illness is critical to rheumatologists, because as Wolfe has taught us, many patients with rheumatic disorders have a little, or a lot, of “fibromyalgianess.”
As we mention regularly here in the community about a combined approach may be considered best in trying to manage Fibro symptoms, see below
Although there is no known cure for fibromyalgia, multidisciplinary team efforts using combined
treatment approaches, including patient education, aerobic exercise, cognitive behavioral
therapy, and pharmacologic therapies (serotonin norepinephrine reuptake inhibitors [e.g.,
duloxetine, milnacipran] and alpha 2-delta receptor ligands [e.g., pregabalin]) might improve
symptoms as well as function in patients with fibromyalgia.
Free Full Text at:
ncbi.nlm.nih.gov/pubmed/214...
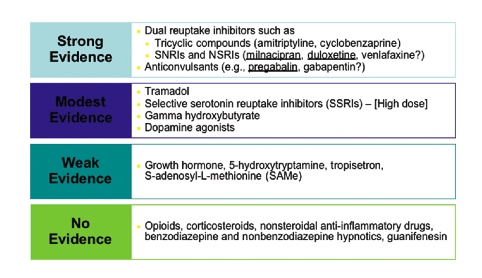
Picture from the same article : Fibromyalgia: An Afferent Processing Disorder Leading to a Complex Pain Generalized Syndrome (2011) by Howard S. Smith, MD1, Richard Harris, PhD2,and Daniel Clauw, MD2