Hi, I wonder if someone could advise me please. sorry if it's too long a story but I feel you need the full picture,
I have been a member of the thyroid group for a while and have found so much help and advice on my thyroid function (or lack of it). My problems started when my mother died very unexpectedly in May 2016. After the initial grief subsided I began to feel very strange, memory loss, couldn't find words I wanted, very cold, tired etc. Having been a very stressed out person all my life (on anti D's for 21 years) due to a dysfunctional upbringing, I thought I would ask GP to check my cortisol serum levels. She also decided to test thyroid and found I needed to increase my levo from 75mg to 100mg. The cortisol levels were high 499 nmol/l (133-537) high but "within range" I then decided to get a salivary test done privately and cortisol was off the chart(high) and dhea low. Saw a private endo who asked GP to test for cushings.....normal result. Since then my serum cortisol has come down to 324nmol/l but nothing is being done about low dhea.
I also suspected my problem could be a b12 def due to my symptoms and the fact that I now realise my mother's symptoms before her death, related to a b12 def. She had peripheral neuropathy, temporal arteritis, low Hg, (3-5),low iron, confusion and after her death I discovered she had brain atrophies. I told my GP and I was tested for I.F and parietal cell abnormalities and B12. On the advice of the admins on the thyroid site I have since had the following tested, to find out why T4 is not converting very well to T3.
Vit D 61 nmol/l . Range 50-200
B12 . 311 ng/l . 180-900
active b12 47 pmol/l . 25.1 -165
folate 4.4 ug/l . >3.8
ferritin 28 ug/l . 15-300
I should mention that I take methotrexate 10mg per week for RA and folic acid 5mg once a week, two days later. Also Naproxen (NSAID) and omeprazole (PPI) to protect stomach lining from NSAID
Two weeks ago, I suddenly found myself very short of breath, even at rest and mentioned it to GP when taking in my active b12 tests for his opinion. He became very concerned, a chest xray was done..clear, an ecg..clear, finger Oxygen 98%. After this he has now decided from my latest bloods that I am borderline B12 def.
I had my first shot yesterday and will have another five in the next 2 weeks then one shot three monthly. He said he has decided to do this for a year!?? He didn't tell me but I have had to educate myself and realise I need co-factors which I intend on taking, Vit D top up to total dose 5000iu as I already get 400iu daily from gp as I have osteoporosis as my mother did as well as R.A. I need a good Vit B complex (Thorne basic B) K2-MK7 and Vit C if I need iron. My queries are:-
1. Is it the lack of B12 that has caused my ferritin levels to drop? Hence shortness of breath. Oxygen measured on finger was 98%
2. Now that I am having B12 shots, will my ferritin come back up to normal because GP didn't think my blood showed any real abnormalities? I didn't receive any advice about taking additional co-factors, minerals, vits. etc
3. Do I need to supplement iron/ferritin and if so how much and what type/brand?
I have been trying to get help with these problems for 18 months and now that I am getting something done about it, I don't want to mess things up.
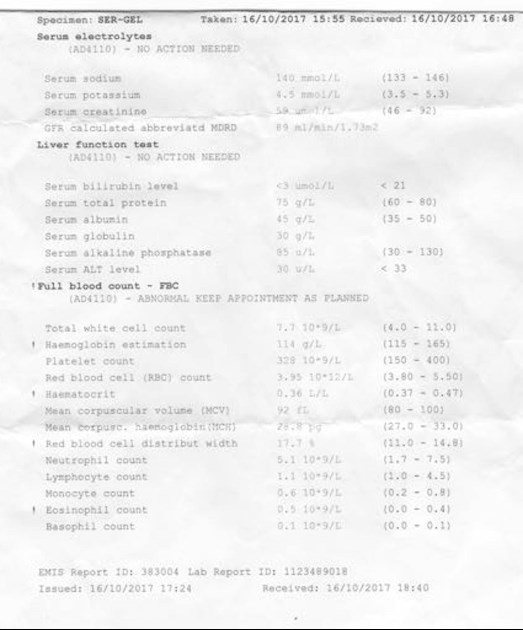
Thank you for reading my story and I would appreciate any help you can give. I am also attaching some test results for bloods taken 16th October this year. My levels have dropped since August but I couldn't upload 2nd picture. It's taken me 2 hours to sort this one out. Sorry print is so light. Thank you so much.
Linda