Does anyone have any ideas what these results mean please?
My history is 3 months of constant watery diarrhoea often with undigested food in it.
It has since stopped as quickly as it began. No bugs found, calprotectin test was 176.
Could it be IBS?
Does anyone have any ideas what these results mean please?
My history is 3 months of constant watery diarrhoea often with undigested food in it.
It has since stopped as quickly as it began. No bugs found, calprotectin test was 176.
Could it be IBS?
Has your doctor not explained the results to you? It seems odd you would get a copy of the report without someone explaining the results.
I agree with jackup, and will be very interested in what your doctors explain about these results
When my upper GI tract has been biopsied by endoscopy clinic (ie during gastroscopy) my biopsy results reports have always read somewhat similarly in that the lab tests on the samples taken revealed chronic inflammation, but also they have identified specific conditiins ie chronic gastritis & chronic oesophagitis with metaplasia of the gastric type.
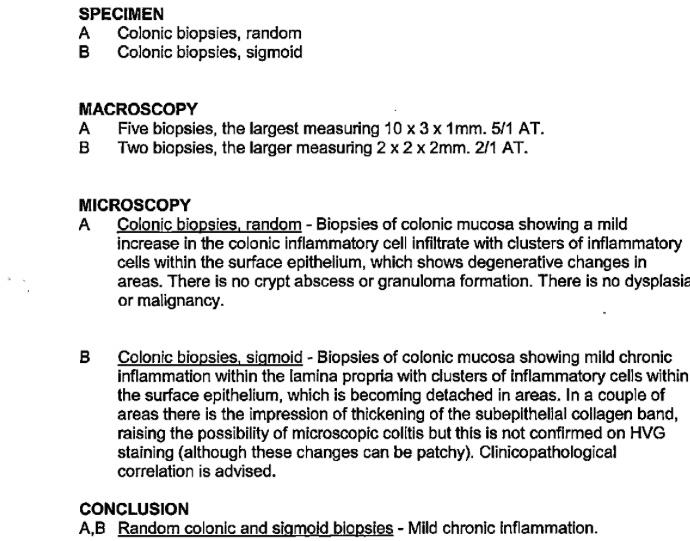
Reading your results, my amateur impression is that the lab is reporting chronic mild inflammation in parts of the colon, but your gastroenterologist is not yet actually interpreting what these lab results signify. I don’t see how these can signify IBS, because although IBS is officially said to be confinded to the large intestine, ie the colon, IBS is not YET officially said to feature actual inflammatory process affecting & changing colon tissues the way your lab biopsy reports seem to me to indicate inflammatory process has affected your colon.
But i’m not an expert...just an informed amateur married to an early onset severe crohns patient of 64, with a sister-in-law also managing severe crohns, and with close friends & family who have colitis, IBS etc. I myself have rare early onset mouth to exit inflammatory process in action due to underlying infant onset immune dysfunction & connective tissue diseases (lupus, sjogrens etc)...and i am now in my 10th month on crohns care protocols due to Intestinal Failure especially affecting my small intestine
If i were in your shoes, i’d see the gastro who ordered your colonoscopy for explanation/interpretation of these results. And if she/he admits these results cannot explain the severity & persistence of your diarrhea, then i’d ask what she/he intends to investigate next, eg, my amateur experience/feeling is that they should possibly be thinking about looking more closely at your small intestine via video capsule endoscopy &/or MRI enterography to see whether the primary cause of your manifestations could be in there
If she/ he says further unvestigations are not indicated, then i’d ask what you should do if another phase of persistent diarrhea sets in
I hope something in all that is useful. And i hope you’ll keep us posted
Good luck, Coco
Thank you very much for your response and taking the time to write your reply which was full of great info. I got my biopsy report from my online Nhs App and haven’t got an appt yet with the consultant who requested it. I did have a US scan on my liver gallbladder pancreas & kidneys about 10 days ago so maybe I will get an appt sent to me soon. It’s interesting that IBS doesn’t show inflammatory properties. I will keep you posted thanks again.
Thanks milly...& you’re v welcome
There is A LOT of debate among gastroenterologists & rheumatologists about whether IBS can involve inflammatory process. So, watch this space! The gastroenterologists at my univ hospital tell me this debate drives them to distraction...but they cannot stop it going on:
I think the confusion especially arises in patients like me whose investigations show too few of the IBD diagnostic criteria relating to crohns or colitis...BUT whose GI tract probs are highly symptomatic & responding positively to the immunosuppressant meds (prednisolone (steroids) etc) we are taking for our autoimmune diseases, (which all feature inflammatory process just about all over our bodies). These meds are the same sort of powerful meds prescribed to crohns & colitis patients
So at the mo, my consultants cannot say i have IBS, but they can’t say i have crohns or colitis, Instead they think i have an unusual form of crohns-like IBD enteropathy caused by my lupus, sjogrens etc, which they cannot label IBS because these GI probs of mine involve inflammatory process which is consistently damped down by my immunosuppressant meds.
Hope that makes some sort of sense...
It seems a bit of a mystery, I haven’t been diagnosed with any auto immune diseases but have had joint pain throughout my body especially my mid and lower back, shoulders ribs and feet. I also get a horrible discomfort in my bladder that flares up at times that is unexplained. Due to all these symptoms I was told i have fibromyalgia? Which I believe doesn’t show up as inflammation.
My aunty has symptoms just like me and she is waiting for an appt with the rheumatologist as her GP suspects sjrogens.
I’ve been on different meds like amitriptyline & gabapentin to help with the fibro but nothing seems to work so I’m taking Duloxetine 60mg now as there has been some good results reported with that. I’ve been on it about 6 months and did wonder if this may have caused my diarrhoea.
V interesting. It’s really good you’re observing your signs & symptoms and aware too of your aunt’s health issues. All this is how you can help rheumatology to help you. Achieving convincing diagnosis & effective treatment plans is a process involving both you & your hp & your rheumatologist. This process can & often does take a few years of investigations & monitoring. The more self-aware you are, the more you can help in this process. I also attend the Lupus UK HealthUnlocked forum where we welcome fibromyalgia patients who wonder whether they may possibly also be affected by other lupus-like autoimmune conditions...if you ever feel like asking about your mix, there are bound to be people there who can help: it’s a very kind, sensible, practical group, closely overseen by wonderful staff at LUK headquarters:
Hello,
I can't say what you results mean but I can say what it doesn't mean...
Calprotecin below 50 is normal. 176, as mentioned, you have inflammation. IBS does not involve inflammation. With IBS calprotectin should/would be normal, below 50.
Inflammation is coming from lower part of digestive tract (stomach, possibly but maybe lower) this could be IBD involving large intestines, or another type of IBD for the small intestinesine, pancreas or a few other things. But before you panic, 176 isn't extreme, ulcerative colitis can easily reach 1500 for calprotecin. It could be a one time thing, never to appear again. It think, not certain here, a reaction to gluten could also raise calprotecin.
Blimey 1500! That is high. I guess my calprotectin test reflects the biopsy result which is low inflammation.
I had the gluten test which was negative as were the 3 fecal tests looking for bacteria etc. Also an elastase test to check my pancreas function which I do not know the results of.
I will just wait and see if I get an appt to see the consultant again to explain if there is a diagnosis or not. I know I’m off the 2 week fast track now which is good so I will have to be patient and wait.
I'll keep my fingers crossed it was just a one off situation.
Not to burst your bubble too much though, at what point during your bout of diarrhea was the calprotecin test....start, middle or end? Near the end, just before the diarrhea stopped might not show the true extent of elevated calprotecin. But since it was self limiting I would think that's a good sign.
You should push for your fecal elastase 1 test results. Keep all of this info and start a file...just to be safe. History is always good to know.