Hi everybody,
I've posted several times lately and I just wanted to ask for advice on thyroid related issues.
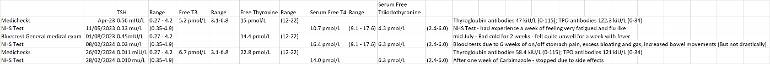
I had COVID 3 times from June 22 - Jan 23 and was symptomatic each time. I did have a diagnosis of Fibromyalgia in 2018 but had been feeling a lot better in 2020 until I got COVID. Above I have documented various tests I've had over the past year or so - my TSH has been a bit low-ish in range until Feb this year where it has dropped significantly bit t4 & t3 still just in range (or just over).
my most results got a diagnosis of hyper (potential Graves but I know this can be incorrect until appropriate testing is carried out) - I started a course of Carbimazole but appeared to have a bit of a bad reaction and stopped after a week.
How important is TSH in terms of symptoms etc? I know it is a 'signal' and not a hormone as such...?
If my t3 & t4 are in range, could my TSH eventually rebalance? would the TSH alone cause symptoms?
Also, is there a lag between symptoms and blood tests? Or does this just apply to those who are medicated?
I am currently not officially diagnosed or medicated and I am awaiting my appointment with endo where I wil have TSH receptor antibody tested (plus others)
Vit D, B12, are in a good range. Ferritin & Folate in range (although folate is low-ish in range).
I’ve been having some intermittent tenderness in my neck / thyroid & symptoms of heightened anxiety, very emotional and depressed. Not leaving the house or getting dressed properly 😔
I just want to try understand what is going on with me and make sure I ask all of the right questions with the endo and hopefully get back to feeling better soon.
Many thanks everybody