Mortality in CKD is dominated by the cardiovascular domain. We will more likely die of a cardio related issue than anything else. We are the highest risk group of all groups for cardio related death. Death for cardio reasons is more likely than our progressing to end stages of the disease: "Expressed another way, persons with mild to moderate (stages 1 to 3) CKD are at higher risk of CV events and CV mortality than they are for progression to ESKD (9,10)."
Here's how one paper title describes vascular calcification:
"The Killer of Patients with Chronic Kidney Disease"
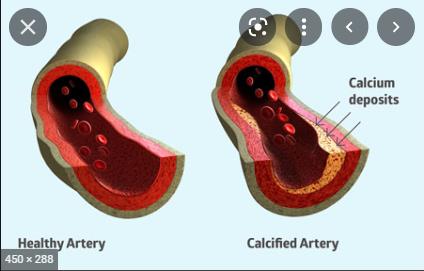
Vascular Calcification is the main cardio disease that kills us. There are others, but this is by far the most significant. We need to prevent / limit VC.
Obviously, calcification requires calcium but whilst we need not to over consume (from whence VC), under consumption leads to bone disorder / fragility. Carbon balance is the term. And like climate change we need to be calcium neutral aka balanced. But how that is achieved??
I figured to open a thread on this specific subject(s) so as to start accumulating current information in one place.
-
SOME RANDOM BITS OF INFO I've picked up as I go:
Vascular calcification (VC) is influenced by, amongst things, vit K2 levels. We don't want to be deficient in it. A significant cause of vitK2 deficiency in CKD is ... diet. We tend to lower consumption of or go off animal products altogether as the disease progresses. Animal products are comparatively high in vitK2 and is where the general population gets it's K2. We also tend to limit green leaf veg (due to higher potassium levels) which also contains comparatively high levels of vitK2. Hence deficiency is common in the CKD population. There is a blood marker that infers/correlates with vitamin K2 status. It's called dp-ucMGP which is a protein that combats vascular calcification when it is activated by vitK2. High levels of dp-ucMGP indicate low levels of vitK2. High because it's not been activated by K2 and therefore isn't doing the anti-calcification job intended for it. Thus can we be potentially serum checked for K2 levels. I gather it not something routinely checked
-
The general population (not CKD) would have a level of dp-ucMGP of something like 300-500 pmol/L. CKD can produce levels in the multiple thousands
-
Link 6 below discusses the various ways in which CV occurs. Here's an interesting piece of it. "Uremic Toxins: compared with serum from nonuremic individuals, uremic serum increases the mineralization (aka calcification) of VSMCs (vascular smooth muscle cells > aka blood vessels) and upregulates the expression of Cbfa1/Runx2 and its target protein OPN". The low/very low protein diet regime aims to reduce serum urea levels. But it's not just urea, it's the other toxins not being filtered out which aren't measured. This is another reason why we need to eliminate uremia - it contributes to VC.
-
Interesting but requiring translating 
"Importantly, as shown by Shanahan and colleagues,19,20,74 changes in VSMC matrix vesicle metabolism induced by hyperphosphatemia and uremia profoundly impair the arterial surveillance normally provided by mural smooth muscle, such as the phagocytic removal of procalcified matrix vesicles and apoptotic bodies."
There are cells that gobble up the crap that would lodge on our blood vessels. Phagocyte - gobbling cell. These cells are the cleaning crew and their work is hindered by hyperphosphatemia and uremia. High phosphorous might be tackled with a med (but it might be allowed to run a bit on the high side). But uremia is tolerated and just goes up and up until you hit the point where the patent side effects of uremia become unbearable/dangerous and you are put on dialysis. But what about the latent work of uremia. Years and years of uremia without manifest symptom = years of uremia hindering the work of the cleaning crew cells protecting your blood vessels. No wonder cardio kills so many before kidneys do.
THE way to tackle uremia is to cut the amount of protein you eat. And so, the pointers towards a low (or supplemented very low ,if need be) protein diet.
Just scanned the 2021 KDIGO guidelines for BP. I was under the impression that systolic was to be managed to <130 (the 2012 KDIGO target as it happens)
Whereas the 2021 guideline has systolic target management at <120. Can't easily see what diastolic ought to be (as I read the 2012 KDIGO and they urged not less than 70, even if it meant letting systolic run higher than optimal (then target was <130)). I imagine diastolic still is important??
-
Lee Hull's "Stopping Kidney Disease" is lite on calcium / VC. The papers he cites talks of VC in the context of its occurance in dialysis. That doesn't illuminate us for early stage approaches. He suggests ( but doesn't show adequately) dietary calcium as harmless irrespective of intake whereas calcium supplements do the harm. This may be the result of absorbability?? Lastly, the role of magnesium levels in offsetting calcium effects. Worth exploring that.
Anyone got any further insights into cardiovascular calcification / bone health whether from dietary, supplement, exercise or drug, etc?
-
LINK 0
A readable enough paper covering the various elements involved and showing the paucity of progress in this area. Indeed, progress in CKD treatment isn't noteworthy. Dialysis has been around since the 60's I gather. ACE/ARB? That it??
sciencedirect.com/science/a...
LINK 1
(Note: oldmangreenes link, the one directly below) is an article written by a naturopath who is also selling a book. Neither is necessarily a mark against but you ought to be aware)
homedialysis.org/news-and-r...
-
LINK2
A scientifiky article with lots of links to papers on the subject. Source of the key message at top of page
karger.com/Article/FullText...
-
LINK 3.
If K2 is beneficial then is naturally there's a kicker (there's always a kicker with CKD). If you're on a plant based diet then some of the sources of K2 will now be denied you (my local Tescos always seems to be clean out of natto) and so, perhaps, deficiency.
medicalnewstoday.com/articl...
LINK 4
A comprehensive discussion doc covering how vit K impacts on different aspects such as the dialysis and transplant populations, as well as early stage
healthunlocked.com/api/redi...
LINK 6
Deatiled paper on the various mechanisms at play that lead to vascular calcification. Bit of a teckkie read but it can be skimmed to get an idea. Interesting info therein
jasn.asnjournals.org/conten...
LINK 7
A readable paper on calcium balance and the downsides of too much (vascular calcification) or too little (bone disorder / oesteoporosis). Found by member 'whats'
ncbi.nlm.nih.gov/pmc/articl...