Hello, I am a 23 year old male who first started experiencing symptoms on July 1, 2016 (about 7 months ago). I was in prime physical condition with 9 hours of outdoor carpentry daily, 3-4 days of calisthenics a week and 3-4 sessions of 30 minutes swimming across a lake and back. I had a history of asthma that required daily medication but had been off everything since MIDDLE SCHOOL with no symptoms despite my career and active lifestyle. I assumed my breathing troubles were in the past.
My diet that winter had been VERY good vegetarian + fruits veggies beans but had suffered a bit in the spring with regular processed foods. My diet was somewhere in between in the summer with boiled eggs and regular fruit but not a ton of veggies (mostly green beans/peas) because of living situation. It should be noted that I had been consuming diet energy drinks regularly in the summer prior to the onset of my condition.
Anyways, one day I was swimming and noticed that I felt like i wasn't getting enough air. I chalked it up to poor breathing technique and returned to shore, but found that I was having catching my breath even at rest. I made an appointment with a doctor that evening to get a rescue inhaler. That friday morning i received the inhaler, the condition worsened over the day with no relief from the inhaler, and I submitted myself to the ER that evening. It's worth noting that my voice was much higher/weaker/and cracky upon the worsening of the SOB.
ER did the normal drill for Asthma and prescribed a 5 day burst of 40mg prednisone and advair. Neither of these prescriptions helped and I spent the 4th of july weekend in bed in a depressed state. I returned to work the following tuesday despite still feeling short of breath and chest pain, but over the course of the work week the condition gradually went away, by the weekend I was back to normal and began my normal routine. However, about a week later the symptoms came back leaving me at home bed ridden again, and I have been struggling with chronic chest pain and shortness of breath ever since.
I returned to the doctor who prescribed a 60mg prednisone burst and taper with albuterol/ipratropium bromide twice daily. This allowed me to return to work for a while but I was still struggling with breathing/chest pain. I was only able to sleep 2-3 hours a night while taking prednisone and was taking a cold shower every hour trying to fall asleep given i felt so hot. Given all this i left my job on august 8th and haven't worked a day since.
Since then I have been through multiple prednisone bursts, tried albuterol, max dosage advair (500/50), and spiriva. The only thing that seemed to ever do anything was the 60mg prednisone and duo neb, the albuterol alone does not help AT ALL and. During september i though the condition was getting better so spent time resting but I was wrong. The chest pain and sob is CONSTANT but ebbs and flows in severity (a decent 3-4 days followed by a bad 2-3 days etc). I quit taking all my medication in January due to its lack of efficacy.
From September - December my diet was terrible given my lack of money and consisted of frozen lasagna/pizza and bananas. Since my acceptance to EBT however my diet has improved drastically.
---SYMPTOMS--
Constant Chest pain/tightness, constant shortness of breath, very slight throat tickle, occasional sensation to cough but infrequent and typically unproductive, more noticable upon exertion but symptoms are present at rest. Upon onset of condition voice was abnormal. I have not been able to do any significant physical activity beyond walking ever since quitting the high dosage prednisone.
--WORK EXPOSURE--
In the months prior was exposed to wood dust/drywall dust to no ill effect. Prior to condition was working almost exclusively outdoors but was exposed to significant bat droppings during a home residing. Exposed to significant mold during rotten boat house demolition (about 2-3 days), and exposed to freshly excavated soil and in an area with a high water table.
--MEDICAL FINDINGS--
Doctors have noted either light weezing or no weezing upon all admissions. With only one doctor noting harsh wheezes in lower right lung in late july. All admissions have shown oxygen levels around 98-99% at rest despite severity of symptoms. Blood drawn on 10/17/16 showed slightly low potassium at 3.1 mEq (ref=3.4 - 5.1 mEq/L) and elevated White blood cell at 13.3 (ref=3.4-10.7, 10**9/L). No differential was done on 10/17/16. When differential was done on 11/3/16 white blood cell had returned to normal at 8.0. Differential did show slightly high percentile of monocytes at 11.2% (ref=2-10%) but absolute count was within the normal range at the time at 0.9 10**9/L (ref=0.3-1.0).
D-Dimer has been done in october and january but showed up normal. On 1/17/2017 another hemogram/diff was done upon admission to the ER with stabbing chest pain on the lower left side which showed high MCHC (mean cell hemoglobin concentration) at 37.1 (ref=31.5-36.5 g/dL). This wasn't present in blood tests done previous to this.
repeat xrays have been mostly normal with the exception of moderate overexpansion. A ct scan of the chest was obtained on 11/30/16 with the findings shown below:
**FINDINGS: No significant peripheral interstitial prominence. No bronchiectasis. No geographic areas of air trapping. There is a 5 mm nodule in the left lower lobe image 209. No acute pneumonitis. No pleural effusion. No pathologically enlarged thoracic
lymph nodes. There is a small amount of thymic tissue seen in the anterior mediastinum. Heart size is normal. No pericardial effusion. Limited imaging of the upper abdomen is unremarkable.**
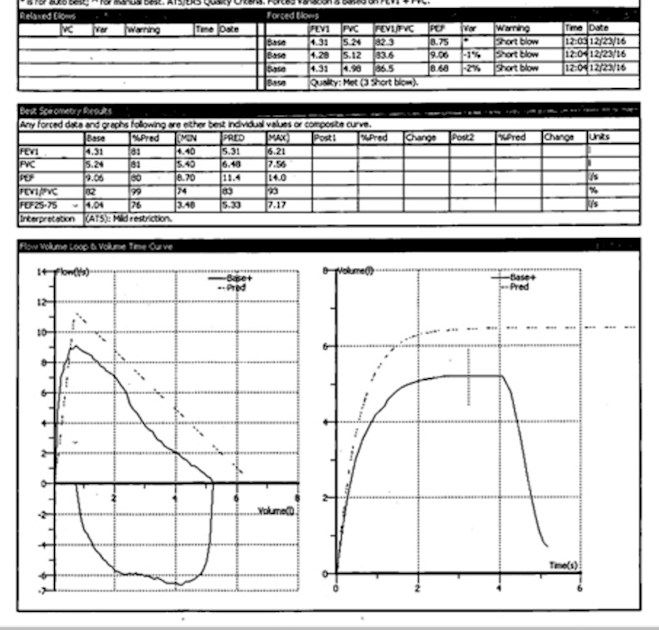
Allergy testing has showed reactions to dogs/cats/dust mites with low severity and very mild reactions to various wood species. Spirometry obtained while taking 60mg prednisone was "normal" but later test indicated "mild restriction" I will add image of detailed spirometry results to this posting. FENO was 15. most recent IGE was low (25 if i remember correctly).
I was recently admitted to pulmonology sometime in January for further investigation. Echocardiagram obtained was normal with mild pulmonic regurgitation. A fungal antibody by cf blood test showed negative for Cocccidiodes, Histoplasma, Blastomyces, and Aspergillus antibodies.
A trip to ER for stabbing chest pain revealed high MCHC but nothing else.
A laryngoscopy was recently done which show inflamed vocal chords and a vocal polyp and I was diagnosed with vocal chord dysfunction. However, it's worth noting that these results were obtained after a bout laryngitis/bronchitis where i had lost my voice due to coughing which was significantly productive (lots of sputum/mucous). Shortly after the laryngoscopy I had a reccurence of the same laryngitis/bronchitis which I have since recovered from. I have been going to speech therapy but the have not found any improvement or relief from my symptoms with the therapy.
After most recent appointment with pulmonary I was instructed to develop a sputum sample, but i have no cough and I'm not sure if I can obtain an adequate one. Would it be worthwhile to request a bronchoscopy from my pulmonologist to obtain better samples?
**MY THOUGHTS/PLEA FOR HELP**
I have lost faith in the Healthcare system and am paranoid that the repeat high dosage prednisone usage and the lack of adequate diet has caused this to last far longer than it should. I am worried that what I am experiencing may be causing permanent damage to my lungs but I am trying to stay optimistic. I am begging for some sort of remedy/potential diagnosis and am willing to try even the most intense therapy regimens with rigorous precision if it will return my life back to normal. I don't want to watch my 20's slip from me.
Thank you all and God bless,
Alex S.