In 2020 my PSA started to rocket up from a 4 at the beginning of the year to a 15.9 at year end. A biopsy was performed. On March 5, 2021 I received the results which indicated adenocarcinoma prostate cancer, with three Gleason score 8s and two 9s. On March 19 of that year a whole-body bone scan was performed and indicated “Abnormal uptake within the calvarium, spine, ribs, sacrum and iliacs compatible with metastatic disease”. A follow up CT scan with and without contrast showed “No compelling evidence of intrathoracic, intra-abdominal or intrapelvic metastatic disease or adenopathy”. By shear luck a relative of mine had a friend that was diagnosed with stage 4 Prostate Cancer. I talked to him and he highly recommended Dr Oliver Sartor at Tulane University. He’s been specializing in prostate cancer treatment for 30 years. My family friend, is still alive 17 years after diagnosis. Conveniently Dr Sartor’s office scheduled an appointment before any local oncologist, Mayo Clinic or MD Anderson. After meeting Dr Sartor I decided to cancel the other appointments and trust in him for the best treatment and advice.
On March 30 I visited Tulane. Bloodwork showed an increase in PSA level to 40. Dr Sartor was able to start me on 1000 mg of abiraterone acetate (Zytiga) and 5 mg of prednisone, that same day. April 9 a local oncologist gave me a 3 month dose of leoprolide acetate (Lupron). Soon thereafter there was a conflict between Dr Sartor and the local oncologist as he wanted me to start on a regime of denosumab (Xgeva). Dr Sartor said if anything, go with Prolia as it’s 60 mg of denosumab every 6 months vs the Xgeva regime which is 120 mg of denosumab every month. The conflict led my local oncologist to recommend I find another local doctor which would be more in tune with Dr Sartor. I whole heartedly agreed and did find a local oncologist that had worked with Dr Sartor in the past.
The good news is my PSA number dropped like a rock. Peeing problems greatly diminished. I could hold it and it actually came out when I wanted it to. The feeling that I have to pee right this second went away. I still wake up 3 or 4 times a night to pee but I can live with that. Pains in my hips and groin has also significantly lessened. I can live with where I am.
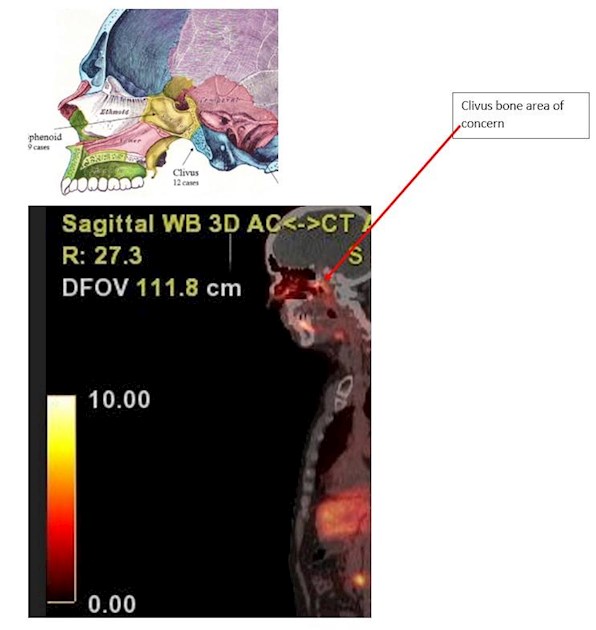
The local oncologist confirmed that we were following NCCN guidelines. Since it had been about 6 months since I started treatment, he recommended I get an Axumin or PSMA PET scan. I chose the later as it’s reported to be more accurate. In October of that year I received a PSMA PET piflufolastat F18 (Pylarify) scan using the latest GE PET scanning machine. I received a CD that shows areas of “uptake”. The follow-on report stated “There is abnormal uptake in the prostate gland diffusely….Maximum SUV value is 5.4 consistent with residual tumor.” And potentially worse “There is a focal area of mild increased uptake in the region of the clivus corresponding with a vague lytic and sclerotic lesion with an SUV value of 5.2”. The doctor also noted mild uptake on several spinal segments, T1, T2, T9, L3 and L4. To me this was a scary read. My follow-up question, is “now what”?
I had a subsequent visit with Dr Sartor’s office. Unfortunately, he had Covid at the time. Later by phone he told me that this is one frame of a movie. You need other pictures to determine if it’s getting better or worse. I asked when should I get another scan. He suggested I not get one until my PSA had increased to 1 or 2. My PSA dropped immediately after treatment started and has tended to be around 0.05 depending on who’s measuring it. Going from 0.05 to 1 or 2 scares me to death. By definition I would have transitioned to the castrate resistant version of this disease where the end is becoming more predictable. Months later I was able to quiz the radiation oncologist whose office set up the scan. He said his recommendation was to stay the course, no radiation or other treatment. I asked my local oncologist and he said the same thing. Not happy with that answer he set me up with another local radiation oncologist and he said the same thing. My follow on question is why do we even get these scans if no one is going to do anything about it?
I had to pay $6200 cash on the spot to get the scan in the first place. Trying to get reimbursed from my insurance company they needed a bill from the PET Scan place which was then jacked up to $8700. The insurance company paid $1700 and now the radiology provider wants me to pay an additional $4700. Something is screwed up here. The insurance company says the max I should owe is $250. You read that right.
For reference I’m included one of my PSMA PET scan images. I would like to add more but it looks like one is the limit. Tear glands and saliva glands light up as they produce PSMA. Liver, kidney and bladder light up as they are trying to remove the radionuclide from my system. Initially the machine initiates a CT scan. If you move the slightest bit the PSMA PET scan won’t line up perfectly. I probably moved my head. Tear and saliva glands are all over the place. Note that my PSA was 0.06 at the time of the scan.
This forum introduced me to Dr Kwon at Mayo Clinic, Rochester Minnesota, who put out three very intriguing youtube videos, youtube.com/watch?v=81iAzYV..., youtube.com/watch?v=Q2joD36..., and youtube.com/watch?v=IEToOBu.... One idea that I totally agree with is to stop talking about palliative therapy and start talking about curative therapy. After my PSMA PET scan I asked about hitting the hot spots with radiation. The local nurse practitioner said they only recommend radiation for palliative care. I’m thinking bring on the morphine. I’m not there yet physically or mentally. Mentally I’m thinking stay on the SOC+AAP curve and maybe after 5 years some better treatment will come along. Going back to the radiation idea, I have a prostate cancer friend that is on the SOC+AAP treatment but he has also received radiation in specific areas. Some of those areas were identified as painful. His PSA dropped after each treatment. Both of the radiation oncologists I talked to said they wouldn’t recommend radiation for me. I gather my cancer is too diffuse to hit and the collateral damage done wouldn’t be worth the effort.
I have a friend that had testicular cancer. It was hereditary. His father had it, and grandfather had it. His grandfather was given 6 months to live. At that time doctors were experimenting with using radiation to “cure” cancer. He agreed to be a guinea pig. The doctors stood him in front of the old time X-ray machines and blasted him for I don’t know how many treatments. He lived another 20 years. He died of a heart embolism due to the radiation. After his death an autopsy was performed and his guts showed significant damage from radiation. But think about it, 20 years of life and a quick death. At this point I would take that deal.
I see Dr Sartor in about a week to get my 6 month Eligard shot. He’s one of the leading experts in LU-177 treatment. To date he hasn’t brought up or suggested I think about that treatment. Do I have to, or should I wait until I’m castrate resistant before experimenting with other therapies? Dr Kwon suggests one consider “triplet” therapy, going after the cancer from different directions before it really has the upper hand. Sounds like a good idea but some information on this forum suggests “triplet” therapy caries more toxicity risk that traditional “doublet” therapy. One of this forums members, Rusland, has been on the Lu-177 + AC-225 therapy and his response is most impressive after he became castrate resistant. Another forum member “Unknown58” is high on, (no pun intended) very much likes, AMG-509.
So again my question is--- PSMA PET scan results received, now what? As I mentioned, I see Dr Sartor in about a week. I intend to quiz him again about:
•Is the PSMA PET scan I took of any use? I’m particularly concerned about clivus bone uptake.
•Should I stay the course until castrate resistant?
•Then do I do chemo, LU177, LU177+AC225, AMG-509 or something else?
As always your informed comments welcome.