Greetings.
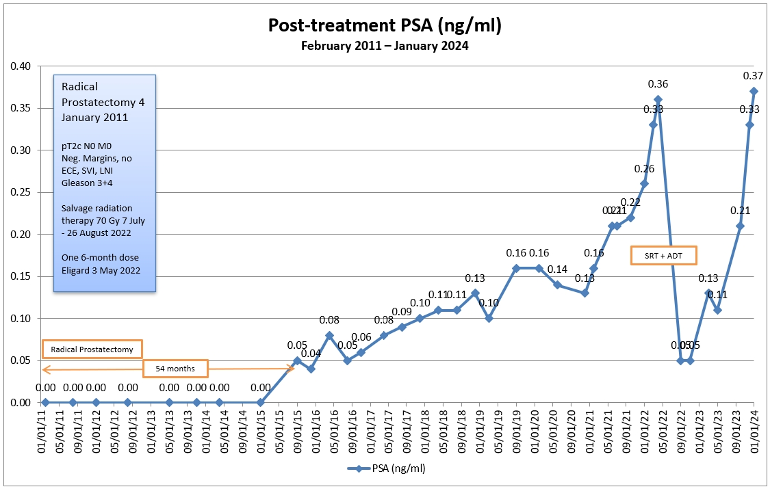
I had a radical prostatectomy that failed and then salvage radiation therapy that appears to have failed as well. A recent PSMA PET scan showed no signs of recurrent prostate cancer or metastases. By way of background:
NOV 2010 - Dx at age 52; positive DRE, Gleason 3+3, PSA 5.0; prostate came out cleanly with negative margins, no ECE, SVI, LNI
JAN 2011 - Radical prostatectomy. pathological Gleason upgraded to 3+4
SEP 2015 - PSA became detectable at 0.05 ng/mL
JUL 2021 - PSA hits traditional biochemical recurrence threshold at 0.21 ng/mL
NOV 2021 - PSMA PET scan with PSA at 0.22 ng/mL; no signs of cancer
MAY 2022 - Six-month dose of Eligard in advance of SRT; PSA at 0.36 ng/mL
JUL-AUG 2022 - 35 sessions of IMRT to prostate bed only
MAR 2023 - PSA 0.13 ng/mL
MAY 2023 - PSA 0.11 ng/mL
OCT 2023 - PSA 0.21 ng/mL, nearly doubling from previous test
DEC 2023 - PSA 0.33 ng/mL
JAN 2024 - PSA 0.37 ng/mL, slightly higher than when SRT was started
FEB 2024 - PSMA PET scan; "no signs of recurrent prostate cancer or metastases"
I'm sure that ADT will be the next step in my future, and I meet with the doctors this week to discuss the recent surge in my PSA and inconclusive PSMA PET. My questions to the group would include:
Is it worth letting my PSA continue to increase to the point where a PSMA PET scan would more likely/able to detect where the cancer is located? That would mean delaying the start of ADT. (Both PSMA PET scans used 68-Ga as the tracer.)
Or is there really little value in knowing where the cancer is at this point and just jump into the ADT?
I'd appreciate hearing any thoughts and insights that may help me have better conversations with my urologist and radiation oncologist.
Thanks!