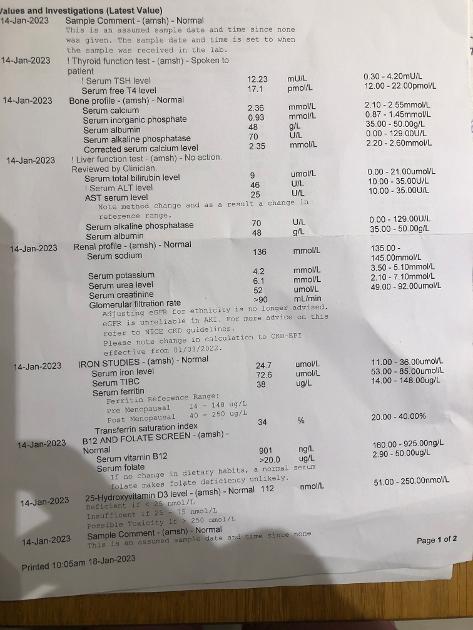
I am on levothyroxine 175 Monday to Friday and 150 at the weekend . My TSH is 12.23 reference range 0.30-4.20. T4 is 17.1 range 12.00-22.00. I was told in October we should try and bring it down to 0.1 so increased by 25 mg Levoth on Fridays. The GP called me last night to say that I have to increase the dose of levo to 200 Monday to Friday and 175 at the weekend . I am unsure that this is the solution. I am seeing a consultant in about a month but with NHS not even bothered to check The whole thyroid panel, it won’t change much ( I’ve seen them in October). I had complete thyroidectomy in 2016 due to cancer. Not sure why TSH went up that much. I also have low ferritin in and supplementing iron and vit c since summer . Brain fog and lacking motivation to finish a project , short fused, fatigue, join pain , put on weight over the tests and difficult to shed it. I did test T3 in summer and it was slightly raised. Will supplementing with T3 if I get hold of it, help? How much does T3 suppl cost on a private prescription in the UK please ? Sorry if it’s all muddled , just feeling really tired and unable to think clearly .
Help please! : I am on levothyroxine 175 Monday... - Thyroid UK
Help please!
Hello Natasha and welcome to the forum :
I am so sorry - you must be feeling awful -
Did you ever have any T3 and T4 readings and ranges taken from when you felt well - so we have bench reading to try and dose back to ?
Has your doctor offered you liquid T4 as it might be more easily absorb and converted into T3 which is the active hormone that runs the body.
I can't see a result or range for T3 and guessing low T3 is the problem since your TSH is way over range as we would expect the TSH to be down at the bottom of the range when optimally medicated.
T4 is inert and needs to be converted in the body into T3 - and we generally feel at our best when our T4 is in the top quadrant of the range as this should in theory convert to a good level of T3 running at around 75% through it's range.
I hope this referral you talk of is through your doctor and on the NHS as you have an obvious issue with the medication current prescribed and the NHS need to resolve this situation for you sooner rather than later.
Thyroid UK the charity who support this forum hold a list of patient to patient recommended specialist who are supportive of offering full spectrum thyroid hormone which considering you have no thyroid function of your own the logical newt step.
A fully functioning working thyroid would be supporting you on a daily basis with trace elements of T1. T2 and calcitonin + a measure of T3 at around 10 mcg + a measure of T4 at around 100 mcg - with T3 being around 4 times more powerful than T4.
In order for any thyroid hormone replacement to work well we do need to maintain a strong core strength and ferritin, folate, B12 and vitamin D at optimal levels and I can see that your ferritin is much too low and suggest this needs building up and maintained at around 100.
Some people can get by on T4 monotherapy :
Some people find they need to add back in that little bit of T3 their thyroid once supported them with :
Others can't tolerate T4 and need to take T3 - Liothyronine only :
Whilst others find their health restored better taking Natural Desiccated Thyroid which contains all the same known hormones as that of the human gland and derived from pig thyroid dried and ground down into tablets referred to as grains.
Thank you for your answer! I don’t have a healthy range as I only tested when unwell only. The letter from October follow up. I was even told that T3 does not need testing , it’s not necessary ( I managed to stay quiet, they think we don’t know anything).
This letter gives a TSH of 2.20 and suggesting a dose increase as your TSH needs to be kept suppressed because of your diagnosis - can't see a date on this letter ??
So why is your TSH now at 12.23 ?
I'm totally confused as to the date sequence of these bloods tests and why the T4 appears to have stopped working.
Do you take any vitamins and minerals that may have interfered with most recent blood test result ?
letter is from beginning of October . I probably took zink, vitDand k, vit B complex at the time , as well as iron. I know to leave a large gap between iron and other medications. I did take Advanced Canfida from Autoimmune, alternating with olive leaf and fluconazole ( nails infection and also found in the stool) for about 2-3 months . I am confused too, GP asked about any recent illnesses , had a viral infection around 20th of December. He said it may be due to that ? I stopped suplim iron from beginning of December , as well as the others for a week prior testing to have more accurate readings . I had a failed reading I guess as the October testing showed higher ferritin( didn’t know to stop before testing).
I did it abroad so range will differ . FT3 was 4.24 range 1.8-4.2 .
When was this Free T3 test and what were the corresponding Free T4 and TSH readings ?
end of July . Anti TG was 15.4 ref <40. FT4 was1.20 ref range 0.8-1.9, TSH 0.539 ref0.4-4. I did have Covid at the time of testing, found out a couple of days later .
So you seemed to be converting back at the end of July :
How were you feeling then - when abroad ?
TSH 0.539 - range 04-4.00 : FT3 4.24 - range 1.80-4.20: Free T4 1.20 - range 0.80-1.90 :
And since August 2022 there's been a gradual decline in your health and well being ?
In October your TSH was at 2.20 and no T3 or T4 readings with a recommendation to increase dose so to achieve a lower TSH :
And now January 2023 we have a TSH at 12.23 a T4 at 17.10 - just 501% through the range and no T3 reading ?
Is this an accurate sequence and picture of what's been going on ?
yes it it . I felt awful for a long time, GP wanted to put me on setraline , I don’t want to that was back in January last year. Then in June I asked for bloods, my ferritin was 11… I felt awful when abroad too, just I kept trodding along because I went there to seek treatment and test my daughter- diagnosed pans/ pandas by Uk private paediatrician and immunologist as NHS don’t treat this either. I also found out I am lactose intolerant so stopped dairy , I was actually feeling better now ( could breath through both nostrils ) then in summer as my daughter got better and life is bearable again? I also found out that I have gastritis that may interfere with what I am absorbing?
Did you get an iron infusion last year to bring up the ferritin ?
Did you self medicate some T3 last summer while away as that could explain your slightly over range last summer ?
Well I would initially ask to try liquid T4 and see if that works any better for you - as i presume with gastritis even T3 Liothyronine tablets may be questionable :
I would ask to rerun the TSH. Free T3 and Free T4 again just to ensure this unexpected high over range TSH isn't just a laboratory ' blip ' :
What has been suggested for the gastritis - are you on any medication for this and could the medication have any bearing on this TSH reading ?
No iron infusion , ferrous fumarate offered by GP which I don’t do well on , replaced with pure encapsulation, biocare iron complex , iron bysglicinate( taking more tablets to make up the dose), I am on iron protocol group now as well. Didn’t take any T3 in summer , now that you said it I took some thyroset from herb and spice from October onwards now and then. Nothing was advised for gastritis, probiotics here and there . I will run tge full thyroid test privately before I go to the appointment… as I did before when unwell ( I remember TSH was at 6is in 2019 , the dose was upped again then…I’ll try to ask for liquid T4 . Thank a million for bothering to read and answer !!!
Thank you for responding !!!
Just thinking on -
since you found out you were lactose intolerant did you mention this to your doctor and was your T4 Levothyroxine medication changed ?
Which brand of Levothyroxine are you currently taking ?
Have you ruled out Gluten intolerance ?
I asked for lactose free brand- Teva.Checked for gluten intolerance( on NHS and abroad)negative , unless is the other type( can’t remember now what is called:(non-celiac gluten intol) that you have to eliminate it all together to see if you feel different - haven’t done that yet.
Always worth trying strictly gluten free diet and/or dairy free
Dairy free since found out that lactose intolerant ( me and my daughter), I am a procrastinator when it comes to bread. I think it’s just a habit I have to break , grew up in USSR when everything was in shortage and would eat bread with anything ( potatoes, rice) just to be full:(. Gluten free was suggested for my daughter that has pans/pandas although tests didn’t reveal an issue with gluten… Will have to do it now :). Thank you and really appreciate that the patients group are more helpful then medical professionals!!!! Most times
Ask GP to repeat the test via another laboratory in case TSH is falsely high.
You can get interference on testing due to mouse 🐁 antibodies!
ncbi.nlm.nih.gov/pmc/articl...
Approx how much do you weigh in kilo
If dose is much higher than guidelines of 1.6mcg levothyroxine per kilo of your weight per day….this suggests malabsorption issues
academic.oup.com/edrv/artic...
Are you taking levothyroxine on its own on empty stomach and then nothing apart from water for at least an hour after
No other medications or supplements within 2 hours minimum
Iron should be at least 4 hours away from levothyroxine and two hours away from other supplements
Vitamin D tablets or gels at least 4 hours away from levothyroxine
Are you currently taking any magnesium
Which brand of levothyroxine are you currently taking
Do you always get same brand levothyroxine at each prescription
private consultation and prescription enables access to Thybon Henning 20mcg tablets T3 via specialist U.K. pharmacies
Cost is 50-60p per tablet
Typical daily dose is 3 x 5mcg doses- cutting 20mcg tablet into 1/4’s
Email Thyroid U.K. for list of thyroid specialist endocrinologists and doctors who will prescribe T3 if clinically appropriate
tukadmin@thyroiduk.org
we need optimal vitamin levels for good conversion of Ft4 to Ft3
Low Ft3 tends to lower vitamin levels, especially ferritin
Ferritin is too low at 38
Aiming for ferritin always over 70 and ideally nearer 100
cks.nice.org.uk/topics/anae...
In all people, a serum ferritin level of less than 30 micrograms/L confirms the diagnosis of iron deficiency
Also See page 7 on here
rcn.org.uk/-/media/royal-co...
Look at increasing iron rich foods in diet
Eating iron rich foods like liver or liver pate once a week plus other red meat, pumpkin seeds and dark chocolate, plus daily orange juice or other vitamin C rich drink can help improve iron absorption
List of iron rich foods
Links about iron and ferritin
An article that explains why Low ferritin and low thyroid levels are often linked
preventmiscarriage.com/iron...
irondisorders.org/too-littl...
davidg170.sg-host.com/wp-co...
Great in-depth article on low ferritin
oatext.com/iron-deficiency-...
drhedberg.com/ferritin-hypo...
This is interesting because I have noticed that many patients with Hashimoto’s disease and hypothyroidism, start to feel worse when their ferritin drops below 80 and usually there is hair loss when it drops below 50.
Thyroid disease is as much about optimising vitamins as thyroid hormones
healthunlocked.com/thyroidu...
restartmed.com/hypothyroidi...
Post discussing just how long it can take to raise low ferritin
healthunlocked.com/thyroidu...
Never supplement iron without doing full iron panel test for anaemia first and retest 3-4 times a year if self supplementing. It’s possible to have low ferritin but high iron
Medichecks iron panel test
medichecks.com/products/iro...
Iron and thyroid link
healthunlocked.com/thyroidu...
Excellent article on iron and thyroid
cambridge.org/core/journals...
Posts discussing why important to do full iron panel test
healthunlocked.com/thyroidu...
healthunlocked.com/thyroidu...
Chicken livers if iron is good, but ferritin low
healthunlocked.com/thyroidu...
Shellfish and Mussels are excellent source of iron
healthline.com/nutrition/he...
Heme iron v non heme
hsph.harvard.edu/nutritions...
Ferritin over 100 to alleviate symptoms
healthunlocked.com/thyroidu...
Low Iron implicated in hypothyroidism
healthunlocked.com/thyroidu...
Ferritin range on Medichecks
healthunlocked.com/thyroidu...
healthunlocked.com/thyroidu...
We have received further information the lab about ferritin reference ranges. They confirm that they are sex dependent up to the age of 60, then beyond the age of 60 the reference range is the same for both sexes:
Males 16-60: 30-400 ug/L
Female's: 16-60: 30-150
Both >60: 30-650
The lower limit of 30 ug/L is in accordance with the updated NICE guidance and the upper limits are in accordance with guidance from the Association of Clinical Biochemists. ‘
1) remember not to take iron at least 2 hours away from thyroid medication. I added desiccated liver capsule to the iron I was taking and it helped 2) it does look like you need a raise, he should have run your free t3 levels also. 3) I am in the US over here we have a test called Reverse t3, do you have that in UK? You can watch some videos on youtube about it, but basically some people they keep raising but their body just increases the reverse t3 so they do not improve. It might be something you want to have tested at least once to see where you are at.
In the mean time, I think raising slowly is better so maybe the 25mcg for two weeks and then get to 50mcg the next two weeks until you are at the desired dosage your doctor thinks you should be on.
however adding t3 is helpful for a lot of people so you may want to consider that, not sure what caused your conversion to have an issue but prior illness may have affected it and maybe it will go back to normal...
Thank you ! I’ll do a private test that includes T3 before my specialist appointment. I often do it as lost faith into this health system.
I’ve looked through and can’t see a mention of this, so hopefully I’m not repeating what somebody else has already said. You said you take a b complex tablet. Did you stop taking it 7 days before the test? It is important to do this as the biotin (b7) in the tablets can skew your results if it’s used in the lab assay.
Hi Natasha76,
This is unacceptable! You’ve had thyroid cancer and the drs are treating you as if you only have an underactive thyroid gland. This is completely wrong and they should be doing a full thyroid blood screen and checking your thyroglobuline levels. I had thyroid cancer and you need to have your TSH seriously suppressed to the bottom of the range or minus to stop the cancer coming back. I was put on Levothyroxine and that didn’t work, and then a mix of Levothyroxine and liothyronine (T3) and that combo didn’t work. Finally, I was trialled on NDT and the result was fantastic! Unfortunately, it was short lived because it was withdrawn and I was back on the synthetics. I jumped the hoops recommended by all the specialists and was finally prescribed NDT after 5 years of arguing and also buying my own NDT from the USA and then that company stopped manufacture and I was back on the prescribed synthetics! Are you still under the care of an oncologist or endocrinologist at a hospital? If you are only being treated by your GP then you need a referral back to hospital.
I am seeing a consultant at oncology clinic on 9th February . I was referred after I complained to NHS abs CCC about my previous GP , I am aware that should be kept under radar for at least 5 years since the diagnosis ( was referred last year after I complained) and had my thyroglobulin checked privately in summer ( was ok) and now recently , the result went straight to them? If I am unwell , I usually do my bloods privately just to make sure. I had to get help from a cousin that is a doctor in France to get advice from an endo, but I ask too many questions and they don’t like that. I saw an endo abroad inAugust , may have to see one here, or a functional thyroid specialist.Thank you very much , I always find the patient groups more caring and knowledgable!!!!
Hi again, do you know what type of thyroid cancer you had? And who told you they only monitor you for 5 years at the hospital? It’s nearly 10 years since my cancer was removed but I’m still under the care of my oncologist at the cancer hospital. My appointments were every 3 months until the covid pandemic hit, and I now have 6 monthly telephone appointments but I have to travel to the hospital for my blood testing and to get my prescription from the hospital pharmacy.
I pulled this off of the web.....Lack of response to levothyroxine therapy occurs due to variety of reasons. Medications such as bile acid sequestrants, sucralfate and others can interfere with absorption, as can taking medication with food, dietary fiber, soy or nutritional supplements containing iron. Gastrointestinal malabsorption, such as from celiac sprue or short bowel syndrome, can decrease absorption of levothyroxine. Increased clearance may occur from phenobarbital, phenytoin, carbamazepine and rifampicin. Weight gain or pregnancy can increase demand.
healio.com/news/endocrinolo...
ICE187 'I pulled this off of the web.....Lack of response to levothyroxine therapy occurs due to variety of reasons.'
Please add a link to the source of the information that you've copied and pasted here, so that members know where it came from.
