Hi everyone, this is my first post (directed from thyroid UK forum) and I have a GP appt today and I’ve just realised I might have a severe B12 Deficiency and possibly even PA!
So was hoping for some quick advice- ive read a lot on this site already so I think I’m justified in thinking this but would be great if someone could let me know if they agree! And direct me in how to tackle this with GP.
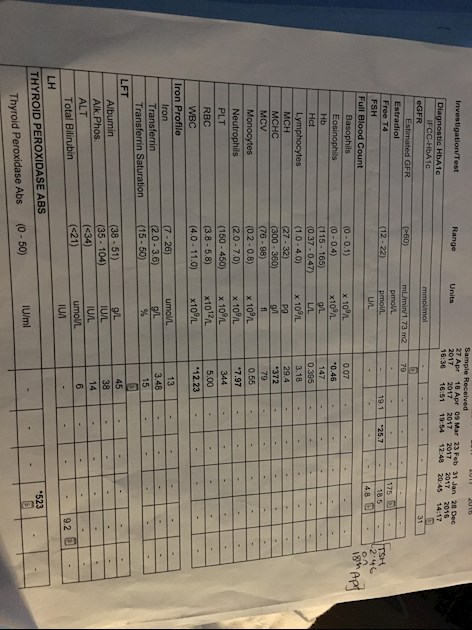
The below blood test results were taken in April whilst I was bleeding heavily (despite being on microgynon- have very heavy irregular periods) and very ill generally.
Bear in mind I was taking folic acid supplements daily and on/off multivitamins with iron supplementation. So my other MCv and MCH were ok and iron.
Main concern: However the MCHC result was quite high (372) and GP said all was fine. Does this point to B12 Deficiency? Or PA? Is it significant enough?
I’ve included a lot of extra info below but obviously don’t expect anyone to read all that! Any help would be grateful - we are due to have frozen IVF in Feb/March and obv I’m keen for everything to be primed before that. thanks in advance ☺️
Some background:
1) I have Polycystic ovaries
2) I’m Autoimmune Hypothyroid- Tx with levothyroxine. (100/125mcg)
TSH :2.9-3.2 atm and free t4: 24 approx
Never tested for free t3.
TPO antibodies 523 (normal range is 0-50)
(I know one autoimmune condition can often cause another/linked to another)
3) Beta thalassemia trait in family. We were tested as children and I believed I didn’t carry the trait but now I’m not so sure if my memory is correct.
- have always had anaemia signs but often not anaemia Via blood tests.
I was severe vit D deficiency last year (undetectable blood range) was given high dose treatment and told to continue with 1000IU daily since (have to say I’ve been lax with that over summer and now)
Symptoms:
- increasingly breathless- always sighing (people comment on it!) short sharp breaths always- have to actively take deep breaths and never feel as if I’m actually getting any oxygen in! (I do have mild asthma but inhalers don’t solve it and it’s not wheezing)
- increasing dizziness and balance problems- vertigo motion sickness (never had these issues before)
Thought this might be ear related as have also been getting earaches-sensitivity to sharp loud sounds, slight tinnitus? And crackling in ear.
Also thought was thyroid related but now thinking PA.
- increased redness around cheeks and nose and excessively dry skin recently (was on holiday recently and a lot of time in pools etc but have increasingly had dry skin for ages)
- sudden diarrhoea (always have digestive issues but it was really bad in April- even went private GP to get stool tests done but never completed it)
- increased swollen tongue and tingling. Pins and needles and ‘crawling sensation on face and legs/arms)