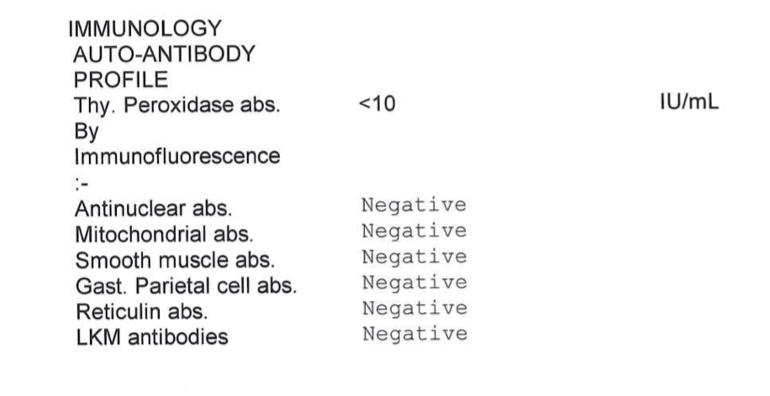
Hi all. I am now SI EOD and have had my iron infusion which is great. I’ve had my autoimmune blood tests back which show I don’t have an autoimmune disease or Pernicious Anaemia (results attached). I’ve been advised that means I have a gut issue which is blocking absorption, I’m keen to get this looked into as I’d like to have the root cause on record with my GP in case anything happens to B12 supply in the future! I know this is probably not the best forum to ask as patients here have PA, but does anyone have any doctor recommendations for testing to find a gastro related cause? Thank you very much.
not PA, next steps: Hi all. I am now SI... - Pernicious Anaemi...
not PA, next steps
Hi AJackson21,
The test for definite diagnosis of PA is highly unreliable. Martyn Hooper had 2 positive Intrinsic Factor tests and 2 negative. (I think that was the ratio in his case). Many people here have not got ‘the gold standard diagnosis’. The test was not performed or whatever. So, I always write PA/B12D to cover all bases.
Now there is over 80 may be 100 autoimmune diseases. This is the Global Autoimmune Institute :-
autoimmuneinstitute.org/res...
Sorry, I have not counted.
With regards to absorption. I do not know where you are in the world but do you have symptoms, heartburn, belching, bloating, poor appetite, stools ? So, :-
1) coeliac/celiac disease, whilst eating gluten for at least 6 weeks. Blood test.
2) H.pylori - stool test.
3) Small Intestinal Breath test - breath test.
All can be ordered by GP. Ask for referral to gastroenterologists for invasive procedures such an endoscopy.
I hope your folate, vitamin D results were ok.
Some of us have low stomach acid but wrongly take antacids. Lemon juice, apple cider vinegar is needed. When we have not got enough acid, we cannot cleave (break down) the essential micronutrients from food. So, we can be deficient in other vital amines and minerals too.
Hope this helps.
Thank you so much for your reply and for taking the time to write that all out! It’s very helpful.
I don’t think I had intrinsic factor tests, I had parietal cell antibodies come back saying I don’t have any. My understanding is that the parietal cell antibodies are present in most people with PA so the fact I don’t have any pretty much rules out PA? The tests I posted above were ordered by Dr Klein at Cambridge Iron clinic who advised me I definitely don’t have PA.
I’m in the UK. I don’t have what I would call heartburn or belching that I know of, after I eat I often get a kind of hiccup type thing afterwards, a bit of what feels like acid reflux, and I feel a bit bloated. My appetite is usually good although sometimes diminishes, I think that’s hormone related though. My main GI symptom is constipation and an ache in my abdomen when I wake up and I haven’t passed a motion in a few days. Those symptoms definitely aren’t my worst but are present.
I had a blood test for coeliac disease a few years ago after eating my normal diet with gluten and it was negative. I’ve always eaten quite a lot of gluten and my symptoms don’t seem to be linked anyway.
I also had low folate so was prescribed folic acid daily and also to take vitamin D daily as it wasn’t tested, as a preventative / to support the B12 I’ve been taking.
Low or high stomach acid is one of the things I was advised it could be. I don’t take antacids, I’ve only had a rennies or two when I’ve eaten something that’s caused me a lot of indigestion, like a spicy curry and that only happens a couple of times a year!
Thank you again for all your help! I was misdiagnosed with ME/CFS so my whole world has been turned upside down over the last few months (in a good but confusing way!) so really appreciate the help getting me on the right track!
Great stuff about Cambridge. Sorry to read about misdiagnosis. Please ensure that your Medical Records are updated and this PA/B12D journey can be an eye-opener.
Dietetics is a specialty in itself and apologies, ask for a referral to one too. Now, for my next trick, I am considering changing from my pyjamas into daywear. 🤣
Just to let you know that several years ago I went to a Pernicious Anaemia Society Conference in Birmingham in 2016 and one of the speakers was Professor John Hunter, consulting physician at Addenbrooke’s. At the time he was leading a research programme into why some patients need more frequent B12 injections than others. So Gastric problems are highly relevant.
youtube.com/watch?v=uaSafQ0...
Here is Prof Hunters talk
To add to Narwhal10 response... Are you taking Proton Pump Inhibitor (PPI)?
Prolonged use of PPI (several years) can cause low stomach acid leading to both B12 and iron malabsorption.
Rexz
I am being treated as if I have PA by my GP even though the IFAB test was negative. I've just had a ferritin infusion and will see what improvement comes about. Researching ferritin deficiency without anaemia, which is what I have, leads me to conclude that I have a chronic absorption problem which deteriorated rapidly with the long term unmonitered use of a PPI. An endoscopy showed fundic polyps, and Heliobacter P which I was treated for with two antibiotics. I don't know whether that worked but HP is bad news for absorption. I now self treat with a combination of probiotics: Symprove, slippery elm, colostrum and aloe Vera to try and heal my digestive system. There have been improvements but an improvement to absorption is so far hard to ascertain. I don't of any tests other than endoscopy and perhaps colonoscopy. Gastric/gut issues are, for me, very much understood by sensation, pain, discomfort etc.
Regarding your antibody test: A negative result does not completely rule out the possibility of pernicious anemia: at least 10% of individuals with pernicious anemia test negative for anti-parietal antibodies.
Would you have some other evidence of autoimmune disease e.g. inflammatory markers etc.? I’ve had lots of autoimmune tests and the only thing that’s come back abnormal is my immunoglobulin M / igM as very high. Interesting that it’s 10%, that’s very high!
The intrinsic factor antibody test is worse- there is about a 50% false negative rate. My B2 was low but I have not bothered with any other tests. It was obvious that B12 was my problem when I went from sleeping 16 hours per day to an energizer bunny with supplements. I had lots of other symptoms as well that cleared up. The sublingual ones worked for many years. But then I got tingly toes. B12 injections cleared that up quickly. I just assume I have PA because B12 is such a miracle drug for me.
AJackson21 A negative result for parietal cells antibodies and intrinsic factor antibodies (did not see that this test was done) means you do not have PA but these tests are "not" conclusive. You could still have B12 deficiency but just not have the antibodies. Medicine doesn't have any tests that can rule out PA, only confirm it..