Understanding how the CLL Tumor Micro-environment (TME) functions is crucial to improving CLL therapy. CLL cells are not as robust as healthy B cells and they rely on their created TME in the nodes and bone marrow for their survival. That's why it's so easy to kill CLL cells with in vitro testing - checking what happens to CLL cells exposed to potential drugs/supplements under a microscope, but then promising treatment candidates rarely work well in human clinical trials; the CLL TME counters the treatment. It's also why smudge cells (CLL cells with ruptured cell membranes) are often reported on our blood tests. Having a high count of smudge cells is actually a good prognostic marker.
Authors from the German CLL Study Group have just published this paper on the role of Macrophages and Nurse-like cells in the TME and how they influence targeted therapies; Impact of leukemia-associated macrophages on the progression and therapy response of chronic lymphocytic leukemia
sciencedirect.com/science/a...
As the paper notes, "The survival of a CLL cell strongly depends on its interaction with diverse factors in the tumor microenvironment (TME)".
Highlights:-
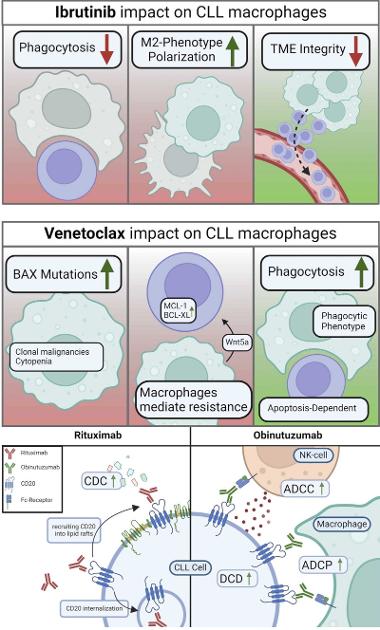
"..CLL remains a complex disease with many patients still experiencing relapse and unsatisfactory treatment responses. CLL cells are highly dependent on their pro-leukemic tumor microenvironment (TME), which comprises different cellular and soluble factors. A large body of evidence suggests that CLL-associated macrophages shaped by leukemic cells play a pivotal role in maintaining CLL cell survival. In this review, we summarize the pro-survival interactions between CLL cells and macrophages, as well as the impact of the current first-line treatment agents, including ibrutinib, venetoclax, and CD20 antibodies on leukemia-associated macrophages."
• Macrophages are important contributors to the progression of CLL.
• Frontline drugs not only target CLL cells but also affect macrophages substantially.
• Macrophages potentially influence the development of treatment resistance.
• Understanding CLL-macrophage interplay can lead to treatments overcoming resistance.
Headings:
1. Macrophages are indispensable supporters of chronic lymphocytic leukemia (CLL) cells
2. The generation and utilization of nurse-like cells (NLCs) have unveiled crucial mechanistic interactions between macrophages and CLL cells
3. Macrophages are strongly influenced by CLL therapy and contribute to therapy resistance
3.1. Ibrutinib and BTK inhibition
3.2. Venetoclax
3.3. Anti-CD20 monoclonal antibodies and the phagocytic role of leukemia-associated macrophages
4. Perspectives and Conclusion
Taken together, macrophages are major contributors not only to CLL progression but also to treatment responses and resistance development. Macrophages are the main actors in mAb treatment and play an important role in responses to several first-line treatment agents. While CLL treatment has advanced substantially over the past decade, resistance cases to these agents are constantly rising. This review underlines the importance of further investigations of macrophage polarization and functions under different treatment regimens. Comprehension of the complex effects of different immunomodulatory drugs on both leukemic cells and bystander compartments such as macrophages, as well as their impacts on the interplay between these cellular factors, may foster novel therapeutic combinations for tumor microenvironment remodeling and improved patient outcome.
Combined figures 2 and 3 from the paper, showing the interaction of ibrutinib, venetoclax with macrophages and rituximab and obinutuzumab with CLL cells respectively, are shown in the attached image.
We've had a few other posts recently regarding the TME;
• Targeting the tumor microenvironment for treating double refractory chronic lymphocytic leukemia posted by newyork917 healthunlocked.com/cllsuppo...
• Nurse like cells (NLC) and cll and monocyte levels posted by bachplayer13
• Latest study improves our understanding of the role the immune microenvironment plays in chronic lymphocytic leukemia posted by CLLerinOz
With thanks to CLLerinOz for bringing this paper to my attention
Neil