In countries where targeted therapies ('brutinibs, venetoclax, obinutuzumab/rituximab) are now available, the remaining reason that FCR (Fludarabine+Cyclophosphamide+Rituximab) is still sometimes recommended for the treatment of CLL is that it can be curative* about 55% of the time - but only if your CLL is IGHV mutated. Unfortunately, the chemo constituents of FCR bring with them around a 10% risk of the subsequent development of Acute Myeloid Leukaemia (AML) or a Myelodysplastic Syndrome (MDS), where your bone marrow increasingly struggles to make blood cells. Also, in countries with universal health care systems (that's nearly all of the world other than the USA), gaining approval for the more expensive targeted therapy treatments relies on evidence that the newer treatments have long term cost and health advantages over BR (Bendamustine+Rituximab) and FCR. Hence this study, Trends in risk for therapy-related myelodysplastic syndrome/acute myeloid leukemia after initial chemo/immunotherapy for common and rare lymphoid neoplasms, 2000-2018 being of interest, particularly for those contemplating whether FCR is worth the risk over more modern treatments.
Abstract: pubmed.ncbi.nlm.nih.gov/374...
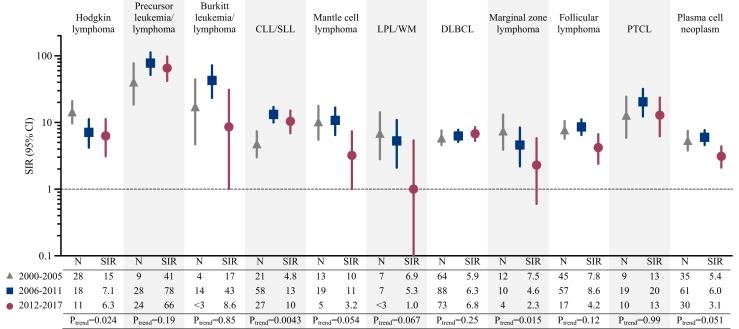
Attached, I've included the plots of the Relative risk for tMDS/AML occurring within 5 years after initial chemo/immunotherapy for a first primary lymphoid neoplasm. (tMDS/AML is the abbreviation for therapy-related MDS/AML). The Abstract Interpretation: Although tMDS/AML risks are significantly elevated after initial chemo/immunotherapy for most LNs, patients treated more recently have lower tMDS/AML risks, except after CLL/SLL. Though rare, the poor prognosis following tMDS/AML emphasizes the importance of continued efforts to reduce treatment-associated toxicity.
If you look at the three 5 year study groups covered in this report, the standardized incidence ratios (SIRs) for CLL/SLL and DLBCL haven't improved, while there has been some degree of improvement in other blood cancers. For CLL, the increased risk of developing tMDS/AML is somewhere between 3 and 20% and still averaging about 10% over the last 5 year period, from 2012 to 2017. Dr Davids noted "a 6.3% cumulative risk of therapy-related myelodysplastic syndrome (MDS)/acute myeloid leukemia (AML)" from the 19 year long term follow up report in his commentary.
* Long term follow-up of those treated with FCR, has shown that if you make to 7 years in remission, your remission is likely to last 20+ years. That is, early FCR recruits that achieved 7 years of progression free survival, have recently entered into their third decade of living without their CLL returning. (CLL researchers are reluctant to say 'cured', but I think most of us would consider surviving 20+ years post cancer treatment as a cure!)
I can't see any justification for Bendamustine+Rituximab (BR) treatment when targeted therapies are available. You don't see this curative effect with BR. We are yet to see if this effect occurs with combination targeted therapies, such as venetoclax plus a BTKi or 'mab therapy; CLL researchers were hopeful that this would be seen, perhaps even with unmutated IGHV CLL, given we don't see the big difference in achievable remission times with targeted therapies between mutated and unmutated folk, but we are still a few years off that 7 year point when remissions became indefinite after FCR treatment.
This is an unlocked post
Neil