This is an important evaluation and insight into how your CLL profile affects your response to VR in relapsed and refractory CLL. Sadly it looks like bad genetics is still relatively bad news in terms of PFS even on VenR.
"In previous analyses of the MURANO study, fixed-duration venetoclax plus rituximab (VenR) resulted in improved progression-free survival (PFS) compared with bendamustine plus rituximab (BR) in patients with relapsed or refractory CLL. At the 4-year follow-up, they report long-term outcomes, response to subsequent therapies and the predictive value of molecular and genetic characteristics."
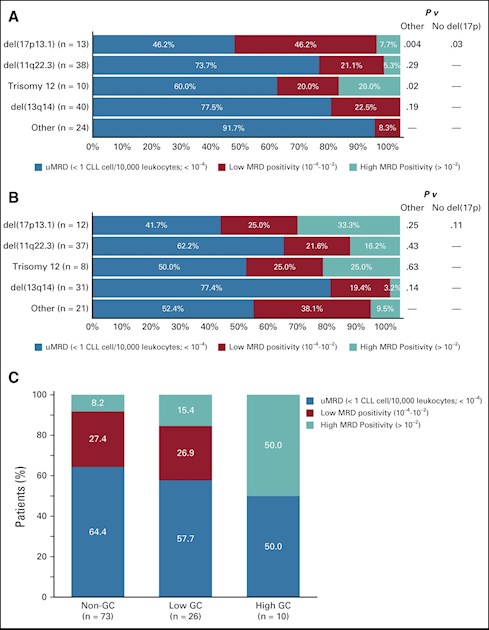
"Undetectable MRD at the end of combination therapy (EOCT) was associated with superior PFS compared with low MRD positivity and high MRD positivity. Patients in the VenR arm who received ibrutinib as their first therapy after progression (n = 12) had a reported response rate of 100% (10 of 10 evaluable patients); patients subsequently treated with a venetoclax-based regimen (n = 14) had a reported response rate of 55% (six of 11 evaluable patients). With VenR, the uMRD rate at end of treatment (EOT) was lower in patients with higher genomic complexity (GC) than in those without GC; higher genomic complexity (GC) was associated with shorter PFS. Higher levels of MRD positivity rates were seen with BIRC3 and BRAF mutations at EOCT and with TP53, NOTCH1, XPO1, and BRAF mutations at EOT."
'Clinically relevant biomarkers predictive of poor response to CIT include unmutated immunoglobulin heavy chain (IGHV) gene, del(17p), mutated TP53, and cytogenetic or genomic complexity (GC).8-11 Targeted therapies overcome the adverse impact of IGHV status, but the identification of biomarkers for targeted therapies is required to guide clinical practice. Specific biomarkers that might have predictive value with targeted agents as well as CIT are certain recurrent mutations and GC. How to define GC is currently under debate. It was recently found that presence of five or more, but not three or more, chromosomal aberrations is an independent prognostic factor with adverse outcome in CLL after chemotherapy. Whether this also holds true for targeted agents is currently unknown.
They concluded that
"The data shows a sustained long-term benefit for fixed-duration VenR in R/R CLL and suggest that extended therapy would be unlikely to prevent early progression. Data for next-line therapy indicate the potential of either ibrutinib or venetoclax re-treatment as a treatment option after progression on VenR. The clinical relevance of the biomarker findings requires validation in further studies.
Efficacy benefits with fixed-duration VenR are sustained and particularly durable in patients who achieve uMRD. Salvage therapy with ibrutinib after VenR achieved high response rates. Genetic mutations and GC affected MRD rates and PFS"
Much more detail here: ascopubs.org/doi/full/10.12...
Jackie