Time for a really specific question that is at the nub of the decision faced by doctors and patients when it is time to initiate first treatment. Does it matter which treatment we choose first?
If you are a younger patient then clearly one of the critical issues is that sadly our disease is rarely cured. As we saw in yesterdays post on response rates and relapse a certain percentage of patients will relapse even on a drug like ibrutinib. Probably eventually we all will (assuming we are young enough to live that long).
See: healthunlocked.com/cllsuppo... for explanation of some of the terms used below.
In my head, as a 47 year old about to start first treatment who is unumutated, I am assuming I will work my way through multiple treatments over what I hope will be say 30 years or more of life.
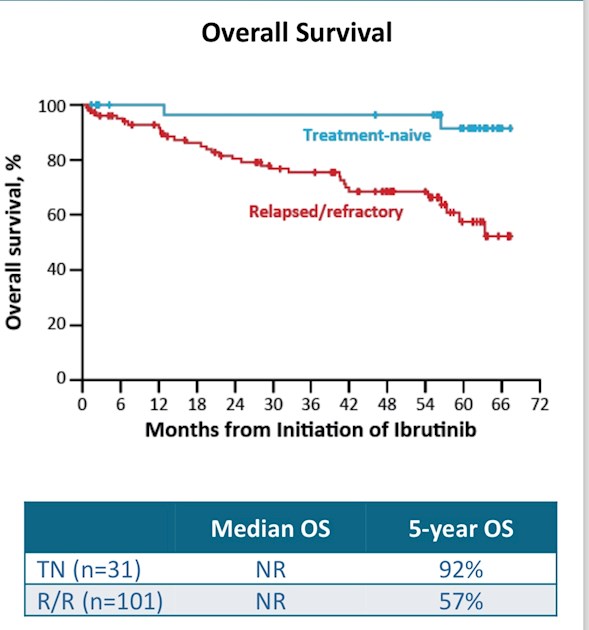
It is clear from the data that ibrutinib was associated with better progression free survival and overall survival in the first-line study than it was in the relapsed and refractory study. (ASH 2016, 1102-03 5-year Update; O’Brien et al)
Initial therapy: Five year Progression Free Survival(PFS): 92%, Overall survival (OS): 92%
Relapsed/Refactory study: 5-year Progression Free Survival: 43% and Overall Survival: 57%.
The graphic attached to this post shows this graphically for overall survival.
On the face of it this would seem to indicate that you should use ibrutinib early in the disease. And an attempt was made to look at this in more detail based on the number of treatments someone has received:
0 prior therapies (n=31) Overall Survival at 5 years 92%
1-2 prior therapies* (n=27) Overall Survival at 5 years 60%
3 prior therapies (n=14) Overall Survival at 5 years 85%
≥4 prior therapies (n=60) Overall Survival at 5 years 47%
There are a number of potential problems with this simple assumption, however.
1. The numbers involved are really very small and so subject to quite a lot of random variation in an older population where some people will die of other unrelated causes. A single chance event death in any of these groups could skew these results (e.g. is it Really likely that people with three prior therapies would do better than those with two?)
2. The paper notes that they only had two patients in the R/R group who had only had one therapy, so we don't really know anything about what would perhaps be the most common strategy if you are not opting for ibrutinib firstline: start with FCR then move to ibrutinib when required.
3. The first-line patients were less likely to have bulky disease, an increase B micro globulin level, and 17p or 11q deletions than the R/R group. Thus the R/R group are a sicker group of patients. And when it comes to the deletions the presence of 17p or 11q was associated with a worse outcome even with ibrutinib use.
4. When we say that ibrutinib appears to work better in treatment naive patients are we simply saying that treatment naive patients do better no matter what treatment they have? Or are we saying that chemo can damage the prognosis of patients with CLL making it harder for ibrutinib to work later down the line?
5. Are we really saying that no matter what the treatment patients with good prognostic markers will do better than those with bad markers? And that the longer the patient has the disease the more likely they are to both progress and die no matter what treatment you are given?
The UK model outside of the FLAIR trial is that everyone with any 17p deletions (no matter how infrequently they are expressed) are assumed to be high risk and not given FCR, but move straight to Ibrutinib. The rest are given FCR, then, anyone who relapses after being given FCR may be given ibrutinib.
Do we know for sure that such a strategy is worse then moving everyone to ibrutinib first line?
It may well be that ibrutinib can rescue effectively patients who relapse on other treatments. Of especial note in the Four Years Follow-up of the RESONATE trial was the fact that it allowed patients during follow up to switch from the comparator (chlorambucil) to ibrutinib. This led to over time the survival curves of the two initial groups of patients to significantly narrow. I.e. patients who moved to ibrutinib were more likely to survive. (Byrd J. et al. Long-term efficacy and safety with ibrutinib in previously treated CLL: up to four years follow up of the Resonate study. Poster presented at the American Society of Clinical Oncology (ASCO) 2-6 June 2017;Chicago, Illinois, USA)
What about those with intermediate or low risk markers? Mutated and Un-muated patients do equally well with relapsed/refractory disease when treated with ibrutinib. The survival curves map almost exactly.
So there is little evidence that patients would do worse on ibrutinib if they had been previously given FCR as an IVGH unmutated person (provided they don't have 17p deletion), although there IS evidence that FCR itself is less likely to give you a long remission if you are not mutated in your IVGH gene.
In the long term follow up of the original FCR study CLL8, half the patients were still being followed up 12.8 years later. Obviously we do not have anything like this long data for ibrutinib. See bloodjournal.org/content/12...
Progression free survival (PFS) at 12.8 years was 53.9% for patients with mutated IGHV but only 8.9% for patients with un-mutated IGHV.
Median PFS (the point when more than half the patients had relapsed) was not reached (NR) for patients with IGHV Mutations but was 4.2 years for patients who were un-mutated.
When it comes to overall survival it is important for younger patients like me to remember that these groups are much older than me. So many of them will die for other reasons. Nonetheless there are differences seen also in overall survival for FCR treatment.
Median Overall survival (the time till when half of the population had died) was 12.7 years
Predictors of death in the study were: age ≥65, IGHV-Unmutated status, B2M ≥4.0, and del(17p).
Median Overall Survival for patients with IGHV-Unmuated was 9.4 years, with 32.2% still alive at 12.8 years. Remember that these patients typically would not have been able to proceed to ibrutinib due to the time of the study.
65.5% of those who were mutated in IGHV were still alive at 12 years (so the median was not reached), and survival was even higher in patients who had a deep remission to MRD-ve patients had an overall survival rate of 87.2% at 12 years vs 56.5% for MRD-positive. There was no effect of MRD status in IGVH un-mutated individuals.
If a patient has low risk (no poor prognosis deletions and mutated) then FCR first-line does look reasonably likely to give them a long remission. The paper also showed that those who experienced a deep remission with no disease detectable in the body were more likely to experience long remissions. And with low risk patients there is even a suggestion that some of them may have been actually cured by FCR.
If patients are intermediate risk then some patients may still get remissions that last for years, but this is far fewer than the low risk group.
So is it better to 'bank' the response you may get from FCR?
Or is it better to use ibrutinib first then move either to FCR or perhaps Venetoclax plus rituximab?
As my CLL specialists told me, the data is clearer for low and high risk patients but perhaps less clear for intermediate risk.
As a result, I do still think the UK FLAIR trial is a very important study. And I can see arguments for and against using each drug first line.
What do you think?
Note this is an unlocked post and so any comments you make could be indexed by google so you are advised not to share personal medical details you don't want other people to know about.