I'm writing this in February about my last blood test a couple of months ago.
I'm always experimenting with my diet to assess its impact on my blood bio-markers.
Most recently, prior to my December blood test, I started having 4 squares daily of 70% cocoa dark chocolate (Lindt).
For the first time, I had an NMR Lipoprofile blood test - this is the most accurate and detailed analysis of blood lipids available.
Here are my results:
All values are in mmol/l unless otherwise noted:
Total Cholesterol: 5.92 (elevated from previous test)
non-HDL: 3.49 (elevated)
LDL-C: 3.05 (elevated)
HDL-C: 2.43 (elevated - but this is good cholesterol so the elevation is desired)
Triglycerides: 0.96 (elevated but still relatively low)
VLDL: 0.44 (elevated but still acceptable)
TC/HDL ratio: 2.44 (elevated but still in optimal range)
TG/HDL ratio: 0.40 (elevated but still in optimal range)
----------------------
So, should I be worried? If a doctor saw these values, and my GP did see them, he would say my LDL is way too high as is my TC and non-HDL. However, my ratios are all still very good and my HDL-C was its highest ever value - a level that is 'out of this world excellent'. I determined that the increased sugar in the dark chocolate was the culprit in elevating my cholesterol values and triglycerides, but also responsible for the increase in the good HDL.
Conclusion? We're not done - the NMR Lipoprofile provided some critical analysis of my LDL-C sub-fractions:
LDL-P (particle number, not cholesterol volume) = 858 nmol/l - this value indicates LOW cardiovascular risk and is in the optimal range of being below 1,000.
HDL-P (HDL Particle number, not volume) = 33 umol/l - this indicates LOW CVD risk and is in the optimal range of being above 30.
Small LDL-P (measures the number of small, highly atherogenic LDL particles) - 162 nmol/l = LOW CVD risk - it is in the desired range well below the cutoff of 527 nmol/l.
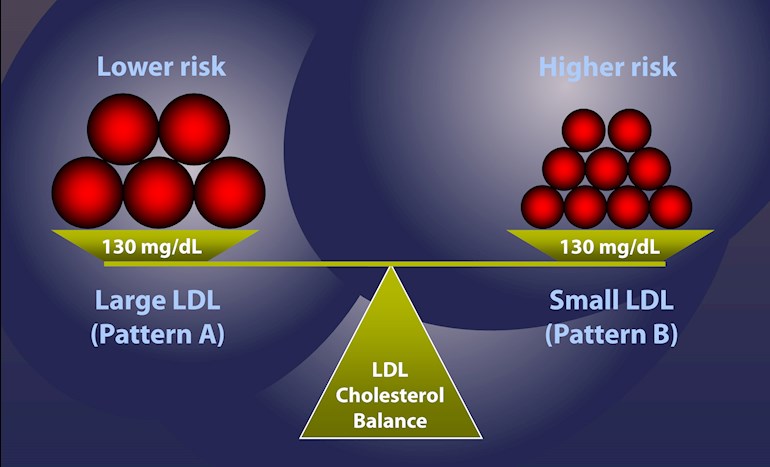
LDL - particle size - (smaller particles are more atherogenic than large particle) = 21.1 nm. = LOW CVD risk - this is in the desired range of being larger than the 20.5 cut off value. A large particle size is classified as 'PATTERN A' and is the desirable pattern, compared to Pattern B, which would be a small particle size.
LP-IR - Insulin sensitivity test - measures the body's level of sensitivity to insulin. If you are insulin resistant it means your body has to produce large amounts of insulin to reduce blood sugar. Those who are insulin resistant 'IR' are typically overweight, have high levels of blood glucose, and are often diabetic. Being Insulin Resistant 'IR', is bad and indicative of high CVD risk. Those who are insulin sensitive 'IS' require only a small amount of insulin to regulate their blood sugar. It is desirable to be 'IS'.
The optimal score is less than 45.
I scored <25, and am therefore 'IS' - insulin sensitive - which is optimal.
Finally, for the 'pièce de ré·sis·tance': Lp(a) considered the most atherogenic component of LDL cholesterol, currently believed by medical science to be genetically pre-determined and un-modifiable with either statins, diet or exercise. High doses of Niacin along with some prescription drugs have been found to lower this value by up to 25% MAXIMUM - therefore due to the inability to significantly reduce - medical science ignores this value and instead focuses on calculated LDL-C for treatment.
The optimal value is <300 mg/l.
My value in February of 2017 was 764 mg/l. Obviously very deflating and representative of elevated CVD risk - but risky only if other bio-markers are also high risk, which mine are not, so I am less concerned, but not happy.
With my brief introduction of vitamin C, lysine and proline (Linus Pauling Therapy), in early October 2017, my Lp(a) declined to 650 mg/l at my October 17th, 2017, blood test - a 15% reduction.
In my recent blood test on December 22nd, my value declined again to 510 mg/l, representing an additional reduction of 22%. In total, from my original test value of 764 mg/l, the current value is a whopping 33% lower! Significantly exceeding the reduction achieved in medical studies using very high doses of Niacin and prescription medicines.
So far, the Linus Pauling Therapy is proving effective. My only problem has been the difficulty of getting enough Lysine dosage daily. I'm only getting 3,000 mg instead of 5,000 mg.
Since this most recent blood test, I have started on Liposomal vitamin C which allows me to get a much higher dosage without any negative side-effects. However I need to focus on getting more Lysine daily (you have to take it in divided doses throughout the day and that is logistically not always easy).
My next blood test is scheduled for March at which time I will also have another angiodefender test, a measure my FMD% score to determine my endothelial function.
In conclusion:
Superficially, the elevated traditional cholesterol markers, likely caused by the sugar in the dark chocolate, would have spooked most doctors into pushing for statins (my GP was not spooked - I have yet to see my cardiologist and he hasn't seen the test results).
However, the NMR Lipoprofile detailed analysis of my LDL composition, clearly shows, that my LDL profile is of LOW CVD Risk. Furthermore, the most critical CVD risk metric, the genetically pre-determined Lp(a) continues to move in the right direction. Finally, I am 'IS' which further indicates LOW CVD risk.
Moving forward - I changed to 85% cocoa dark chocolate, and reduced consumption from 4 squares per day to 2 squares per day.
We will see at my next test the impact of my modifications both dietary and supplementation-wise.
What can YOU conclude from all this - a detailed analysis of your LDL can mean the difference between a doctor pushing for statins or not. It can mean the difference between the anxiety of elevated cholesterol and the calm of knowing the elevated cholesterol doesn't imply higher risk. You should pay for your own NMR Lipoprofile to let you determine your real risk - not that determined by the standard lipid profile. Most doctors are not trained in understanding the NMR Lipoprofile and won't have a clue. You have to take personal responsibility to learn about your real risks.
If you're in the UK, you can find more information about the NMR Lipoprofile test here: invivoclinical.co.uk/invivo...
Stay tuned.

 I've been focussing on getting my thyroid hormones optimal, which has actually brought my total cholesterol down from 9.4 to 7.2 in three months, but was floored by my Lp(a) results, and also the Lp-PLA2 plac test results. I've saved all the info you've given into a word doc and will have a good read through tomorrow when I'm a bit more with it! Thanks again, and it's really great to hear about your success with this
I've been focussing on getting my thyroid hormones optimal, which has actually brought my total cholesterol down from 9.4 to 7.2 in three months, but was floored by my Lp(a) results, and also the Lp-PLA2 plac test results. I've saved all the info you've given into a word doc and will have a good read through tomorrow when I'm a bit more with it! Thanks again, and it's really great to hear about your success with this