Hello, I am wondering you could share your knowledge with me please. I have a healthy, living child who is 2y/o, but I have recently had 3 miscarriages (Oct 2022 6+4, Jan 2023 8+6, and last weekend at 7w). I have MTHFR compound heterozygous, but I was on baby aspirin and a bioavailable prenatal with folate.
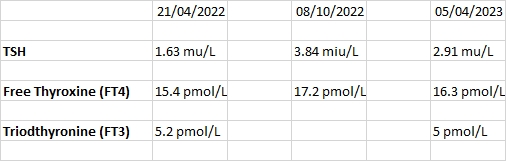
I have done 3 private thyroid tests, results copied here (but I can't seem to move them to a good place!). These results are in normal ranges but I know that for trying to conceive and pregnancy, the TSH should be below 2.5 - this is about all I know. I keep reading things about hypo and hashimotos - I don't think I am there yet, or am I? I was about to order a TPO test - do you recommend? I figured that was the best/only way to determine if it was autoimmune drive? I don't just want to take medication if I don't have to - if I can do something to change it.
Can I manage this naturally? Should I be taking thyroid support supplements? I have been reading this forum and I am considering working on my adrenals then thyroid? The midwives supporting me didn't realise the importance of the thyroid, but the consultant said they will rerun TSH and if it is higher they would start me on low dose thyroxine (I've also read a lot about how this will need checking regularly if I get pregnant again).
This is a bit of a jumble, I'm sorry. Please help if you can!