So at my last GP appt to review all my results, 21 months of blood tests* since the multinodular goitre was discovered in May 2021, the GP said I do not have primary thyroid and I need to let it go, he believes my symptoms are carers burnout.
I raised secondary/central thyroid and we seemed to reach a compromise in doing one last test to check my adrenal function was tested because I'm so fatigued. NHS is a blood test (GP referred but not yet done), I said I would do an adrenal saliva test too.
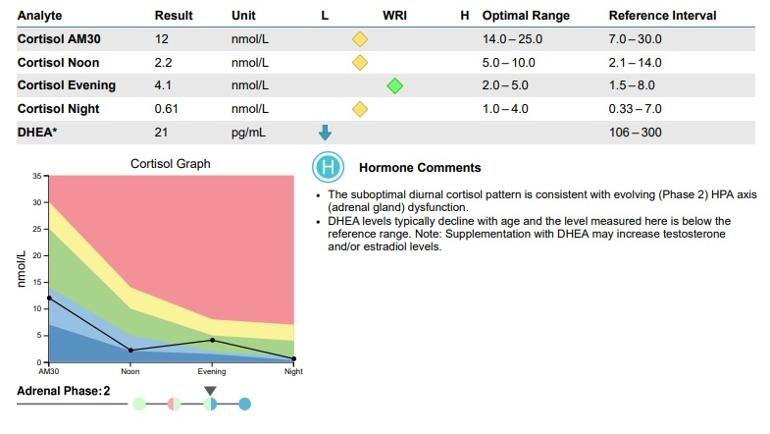
Results are in and cortisol is low 3 out of 4 points as is DHEA.
What should I be pushing for next please?
Thank you so much, you've all got me this far!
* I have multitude of symptoms and feel really unwell which is why I have persisted but until the numbers fit into a box, I cannot be referred to endocrinology.
Symptoms include: debilitating insomnia, fatigue, brain fog, cognitive issues (finding words, memory), aching muscles, neck and back pain, cold, palpitations, nightime anxiety/panic, digestive issues, weight gain. Iron, vitD and vitB12 are low and being treated. Gastro issues like coeliac ruled out by blood test and checked/biopsy during endoscopies. Cholesterol normal.
I take HRT; low-dose Amitripyline for insomnia; Tranexamic Acid for menstrual blood loss; VitD3 softgels, B complex, triple Magnesium & VitK2MK-7 all recommended here.