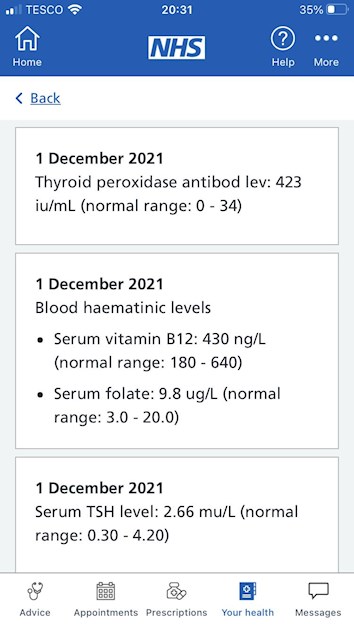
I have just received my latest thyroid tests. TSH level previously was 2.75, so has decreased slightly. Taking B12 supplements. T4 T3 wasn’t deemed necessary even though requested. Antibody reading is up though. Observations appreciated, thanks.
Latest results after Levi increase : I have just... - Thyroid UK
Latest results after Levi increase
Looking at previous posts
You were (finally) got levothyroxine increased from 25mcg to 50mcg 5 months ago
50mcg levothyroxine is only the standard starter dose of levothyroxine
How do you feel?
Your results suggest you need next 25mcg dose increase in levothyroxine
Bloods should be retested again in 3 months
TSH should be under 2 as an absolute maximum when on levothyroxine
gponline.com/endocrinology-...
Replacement therapy with levothyroxine should be initiated in all patients to achieve a TSH level of 0.5-2.0pmol/L.
NHS England Liothyronine guidelines July 2019 clearly state on page 13 that TSH should be between 0.4-1.5 when OPTIMALLY treated with just Levothyroxine
Note that it says test should be in morning BEFORE taking levothyroxine
Also to test vitamin D, folate, B12 and ferritin
sps.nhs.uk/wp-content/uploa...
Graph showing TSH in healthy population
web.archive.org/web/2004060...
Aim is to bring a TSH under 2.5
UK guidance suggests aiming for a TSH of 0.5–2.5
gp-update.co.uk/SM4/Mutable...
guidelines on dose levothyroxine by weight
Even if we frequently don’t start on full replacement dose, most people need to increase levothyroxine dose slowly upwards in 25mcg steps (retesting 6-8 weeks after each increase) until eventually on, or near full replacement dose
NICE guidelines on full replacement dose
nice.org.uk/guidance/ng145/...
1.3.6
Consider starting levothyroxine at a dosage of 1.6 micrograms per kilogram of body weight per day (rounded to the nearest 25 micrograms) for adults under 65 with primary hypothyroidism and no history of cardiovascular disease.
Also here
cks.nice.org.uk/topics/hypo...
gp-update.co.uk/Latest-Upda...
Traditionally we have tended to start patients on a low dose of levothyroxine and titrate it up over a period of months. RCT evidence suggests that for the majority of patients this is not necessary and may waste resources.
For patients aged >60y or with ischaemic heart disease, start levothyroxine at 25–50μg daily and titrate up every 3 to 6 weeks as tolerated.
For ALL other patients start at full replacement dose. For most this will equate to 1.6 μg/kg/day (approximately 100μg for a 60kg woman and 125μg for a 75kg man).
If you are starting treatment for subclinical hypothyroidism, this article advises starting at a dose close to the full treatment dose on the basis that it is difficult to assess symptom response unless a therapeutic dose has been trialled.
BMJ also clear on dose required
Here is the bit D results previously done I’m not taking a supplement for this. Do I need to?
Impressively good vitamin D if not been taking vitamin D
U.K. Government advice is for everyone to supplement vitamin D October to April
gov.uk/government/news/phe-...
Test twice yearly via NHS private testing service when supplementing
Vitamin D mouth spray by Better You is very effective as it avoids poor gut function. There’s a version made that also contains vitamin K2 Mk7
amazon.co.uk/BetterYou-Dlux...
It’s trial and error what dose we need, with hashimoto’s we frequently need higher dose than average
Vitamin D and thyroid disease
Looking at previous post…..Did you get vitamin D tested ?
What vitamin supplements are you currently taking
NHS Guidelines on dose vitamin D required
ouh.nhs.uk/osteoporosis/use...
GP will often only prescribe to bring vitamin D levels to 50nmol. Some areas will prescribe to bring levels to 75nmol or even 80nmol
leedsformulary.nhs.uk/docs/...
GP should advise on self supplementing if over 50nmol, but under 75nmol (but they rarely do)
mm.wirral.nhs.uk/document_u...
But with Hashimoto’s, improving to around 80nmol or 100nmol by self supplementing may be better
pubmed.ncbi.nlm.nih.gov/218...
vitamindsociety.org/pdf/Vit...
Test twice yearly via NHS private testing service when supplementing
As you know from previous post
High thyroid antibodies confirms autoimmune thyroid disease also called Hashimoto’s
GP should have done coeliac blood test…….have they ?
Are you now on strictly gluten free diet?
you have high antibodies this is known by medics here in UK as autoimmune thyroid disease.
Technically it’s Hashimoto's (with goitre) or Ord’s thyroiditis (no goitre). Both variants are autoimmune and more commonly just called Hashimoto’s
Hashimoto's frequently affects the gut and leads to low stomach acid and then low vitamin levels
Low vitamin levels affect Thyroid hormone working
Poor gut function with Hashimoto’s can lead leaky gut (literally holes in gut wall) this can cause food intolerances. Most common by far is gluten. Dairy is second most common.
According to Izabella Wentz the Thyroid Pharmacist approx 5% with Hashimoto's are coeliac, but a further 80% find gluten free diet helps, sometimes significantly. Either due to direct gluten intolerance (no test available) or due to leaky gut and gluten causing molecular mimicry (see Amy Myers link)
Changing to a strictly gluten free diet may help reduce symptoms, help gut heal
Before considering trial on gluten free diet get coeliac blood test done by GP FIRST just to rule it out
lloydspharmacy.com/products...
If you test positive for coeliac, will need to remain on gluten rich diet until endoscopy (officially 6 weeks wait)
If result is negative can consider trialing strictly gluten free diet for 3-6 months. Likely to see benefits. Can take many months for brain fog to lift.
If no obvious improvement, reintroduce gluten see if symptoms get worse.
chriskresser.com/the-gluten...
amymyersmd.com/2018/04/3-re...
thyroidpharmacist.com/artic...
drknews.com/changing-your-d...
restartmed.com/hashimotos-g...
Non Coeliac Gluten sensitivity (NCGS) and autoimmune disease
ncbi.nlm.nih.gov/pubmed/296...
The predominance of Hashimoto thyroiditis represents an interesting finding, since it has been indirectly confirmed by an Italian study, showing that autoimmune thyroid disease is a risk factor for the evolution towards NCGS in a group of patients with minimal duodenal inflammation. On these bases, an autoimmune stigma in NCGS is strongly supported
ncbi.nlm.nih.gov/pubmed/300...
The obtained results suggest that the gluten-free diet may bring clinical benefits to women with autoimmune thyroid disease
nuclmed.gr/wp/wp-content/up...
In summary, whereas it is not yet clear whether a gluten free diet can prevent autoimmune diseases, it is worth mentioning that HT patients with or without CD benefit from a diet low in gluten as far as the progression and the potential disease complications are concerned
restartmed.com/hashimotos-g...
Despite the fact that 5-10% of patients have Celiac disease, in my experience and in the experience of many other physicians, at least 80% + of patients with Hashimoto's who go gluten-free notice a reduction in their symptoms almost immediately.
hypothyroidmom.com/how-to-l...
Eliminate Gluten. Even if you don’t have Hashimoto’s. Even if you have “no adverse reactions”. Eliminate gluten. There are no universal rules except this one.
Thanks once again for a very thorough reply. I’ve been gluten free for over 12 months now and find its helped with the swelling of the goitre I have. I’m taking bile acid tablets too as I have previously had my gall bladder removed and have low stomach acid. Taking these have also helped with constipation. I have an End appointment on Wednesday so I will check the B12 dosas I’m taking and also ask for increase in Levo. After the initial increase to 50 I feel so much better, didn’t realise how bad things were before!