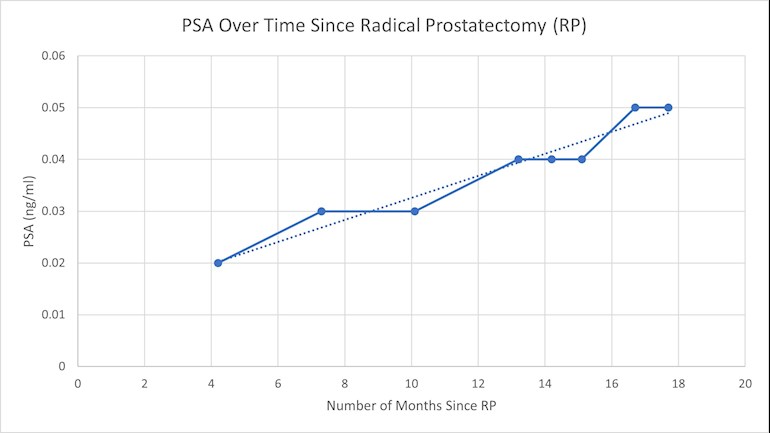
I had my radical prostatectomy (RP) on 6/3/2019. Given my pathological results (see below for details) and the definite trend in my PSA levels over the last 18 months (see graph below), my surgeon now thinks I should pursue early salvage radiation therapy and I agree, but now trying to decide on the best option for salvage treatment. I have met with a RO who does pencil beam proton therapy and a RO who does IMRT both in San Diego. I have a video conference setup for Friday with Dr. Kishan from UCLA to discuss more salvage options including possible ADT. I am trying to prepare for the consultation. Any suggestions on questions I should be asking? I know there are many options for salvage treatments I have been reading about on this forum besides IMRT and proton like SBRT, VMAT, Hypofractionated radiotherapy, HIFU, Cyberknife, real time MRI guided radiation therapy, Elekta, etc. I know this list is incomplete and probably has things that don't apply, but I am only beginning to learn about them and would like ideas. Thanks for any suggestions or thoughts you have. I want to take full advantage of my time with Dr. Kishan.
Here is my history with my prostate, if it matters. I know there is important information in the pathologic diagnosis which is below but not sure which information in that list is the most critical.
Short version of history:
Prostatitis in spring 2014 went to ER and once to doctor office for catherization because could not urinate. Infection went away after a month but PSA was at 5.8 so had biopsy (4/7/2014) which showed no evidence of malignancy. Stayed on active surveillance. MRI guided biopsy on 12/6/2017, found Gleason 3+3 tumor suspicious (PI-RADS 4) lesion in the middle/left transitional zone in the anterior, Clinical T stage: T1c. Repeat MRI guided biopsy on 1/9/2019 with a PI-RADS 4 lesion in the left anterior transition zone and Gleason 3+4 prostate cancer in 4/6 cores on the left apex lesion, as well as 3/6 cores on the left anterior transition zone targeted lesion. Decided in spring of 2019 to RP. Pre surgery PSA 8.3 (graph of all PSAs in graph below).
Details of final pathology from RP below, this is the short version: Adenocarcinoma of the prostate, Gleason score 4+3=7, Grade group 3
. Involving the right
lateral, right posterior medial, left base and left posterior lateral of the prostate (pT2N0). Percentage of pattern 4: 90%, Percentage of pattern 5: 0%. No Intraductal Carcinoma (IDC) identified. Estimated percentage of prostate involved by tumor: 30%. No Extraprostatic Extension (EPE), Urinary Bladder Neck Invasion, or Seminal Vesicle Invasion identified. Margins: Involved by invasive carcinoma, limited (<3 mm). The left apical margin is very focally positive for tumor. The right apical and bladder neck resection margins are negative for tumor.
Detailed history:
February 2014 could not urinate which was supposedly the result of bacteria infection (prostatitis) and ended up in the ER to get a catheter. Took medication for infection (Flomax and Cipro Adovart), finally went away. Learned how to self-catheterize in case needed to but never came back. Urologist did a DRE which was abnormal and prostate volume was 70 cc. PSA prior had been 5.8 so ordered biopsy.
TRUS prostate biopsy on 4/7/2014. Biopsy showed no evidence of malignancy. Had granulomatous which was attributed to the prostatitis and retention. Weaned off the Flomax and Finasteride. Stayed on active surveillance.
March 2015 PSA 5.2.
September 2015 PSA 4.6
September 2016 PSA 5.2
April 2017 PSA 5.5
September 2017 PSA 6.2
Diagnostic Prostate MRI 11/3/2017.
Targeted MRI guided in bore biopsy of an left apical transitional zone lesion on 12/6/2017.
Findings: Tumor suspicious (PI-RADS 4) lesion in the middle/left transitional zone in the anterior Clinical T stage: T1c; % Positive cores 34%; Gleason 3+3, AUA Risk Low. Prostate volume 84.2 cc. PSA Density 0.074 Ng/cc. Central zone no suspicious lesions. T2 slice #24 (left transitional zone, anterior medial prostate within the apex at 1pm. PIRADS 4 lesion left anteromedial transitional zone. High suspicion for malignancy. No evidence of extracapsular extension or metastatic disease.
Continued active surveillance.
March 2018 PSA 6.2
April 2018 PSA 5.6
August 2018 PSA 6.1
November 2018 PSA 7
Diagnostic Prostate MRI 12/3/2018. Demonstrated a new PI-RADS 4 lesion in the left anterior transitional zone. This is a repeat MRI of the apical transitional zone lesion as well as of the new lesion in the left anterior transitional zone. Volume 90.2 cc. PSA density 0.08 Ng/cc. Central zone normal. Transitional zone: transitional zone T2 signal is heterogeneous with matched areas of restricted diffusion and focally increased perfusion that are not clearly suspicious on T2-weighted imaging and are consistent with changes from BPH.
Targeted in-bore MRI guided biopsy 1/9/2019 of the previously biopsied left apical transitional zone lesion (biopsied: 12/6/2017) and the new left anterior transitional zone lesion.
Findings:
A - Prostate, left transitional zone, anterior, core needle biopsies: Prostate adenocarcinoma, Gleason 3+4 involving 13 of 80 mm (3 of 6 cores)
B- Prostate, left transitional zone, apex, core needle biopsies: Prostate adenocarcinoma, Gleason 3+4 involving 41 of 82 mm (4 of 6 fragmented cores)
Contiguous perineural invasion identified
Comment: Pattern 4 represents 5% of the tumor in both biopsy sites.
FINAL PATHOLOGIC DIAGNOSIS: 6/6/2019 (after Radical Prostatectomy)
A: Fat, anterior prostate, excision:
-Benign fibroadipose tissue.
B: Lymph nodes, right pelvic, dissection:
-Eight lymph nodes with no malignancy identified (0/8).
C: Lymph nodes, left pelvic, dissection:
-Nine lymph nodes with no malignancy identified (0/9).
D: Prostate, radical prostatectomy:
-Adenocarcinoma of the prostate, Gleason score 4+3=7, involving the right
lateral, right posterior medial, left base and left posterior lateral of
the prostate (pT2N0).
-No extraprostatic extension identified.
-The left apical margin is very focally positive for tumor, see comment.
-The right apical and bladder neck resection margins are negative for
tumor.
-No angiolymphatic invasion is identified.
-The seminal vesicles are negative for tumor.
-See synoptic report.
COMMENT:
PROSTATE GLAND SYNOPTIC REPORT: Radical Prostatectomy
Procedure: Radical prostatectomy
Prostate Size:
Weight: 100 g
Size (centimeters): 6.0 x 6.0 x 5.5 cm
Histologic Type: Acinar adenocarcinoma
Histologic Grade: Gleason Pattern
Primary Gleason Pattern: Pattern 4
Secondary Gleason Pattern: Pattern 3
Tertiary Gleason Pattern: N/A
Total Gleason Score: 7
Grade Group: Grade group 3
Percentage of Gleason Patterns 4 and 5 (applicable to Gleason score ?7):
Percentage of pattern 4: 90%
Percentage of pattern 5: 0%
Intraductal Carcinoma (IDC): Not identified
Tumor Quantitation:
Estimated percentage of prostate involved by tumor: 30%
Extraprostatic Extension (EPE): Not identified
Urinary Bladder Neck Invasion: Not identified
Seminal Vesicle Invasion: Not identified
Margins: Involved by invasive carcinoma, limited (<3 mm)
Focality: Unifocal
Location of Positive Margin: Left apical
Treatment Effect: No known presurgical therapy
Lymphovascular Invasion: Not identified
Perineural Invasion: Present
Extranodal Extension: N/A
Pathologic Stage Classification (pTNM, AJCC 8th Edition)
Primary Tumor (pT): pT2: Organ confined
Regional Lymph Nodes (pN): pN0: No positive regional nodes
Number of Lymph Nodes Examined: 17
Number of Lymph Nodes Involved: 0
Additional Pathologic Findings:
High-grade prostatic intraepithelial neoplasia (HGPIN)
Nodular prostatic hyperplasia
Ancillary Studies: Not performed
Comment: The left apical margin in this specimen is very focally positive
for prostatic carcinoma. However, the anterior prostate fat is negative for
the tumor. Therefore, the real final resection margin could be negative.
Clinical correlation is recommended.