I started Zanubrutinib April 24th, by 5th day noticed painful finger spasms, 7th day got large dark hematoma (brusing not new but larger size & darker color). Bloodwork showed Hgb 10.8-9.8; Plts 80s-118, WBC 80s-108. I noticed a decrease in the size & number of lymph nodes in my neck, arm pits & upper abdomen. I was fatigued & took more naps. By mid 2nd week my body was aching all over & I thought getting back to my workouts would relieve the pain. I walked on the Treadclimber 45min Day 12. Day 13 I road my Stationary Bike for 60min. Chestpain twinge noted on my deceleration. I thought it just a muscle pull/spasm so I stretched & cooldowned on my vibration plate. After 3hrs Chestpain still there & off to ER. Long story short I have Pleurisy, friction between Left Lung Lobes = Left Pleural Effusion r/o Atelectasis vs Pneumonia. Treatment Plan; Proventil Nebulizer 4X per day as needed, Doxycycline 100mg po 2X per day x 1 week, Prednisone 40mg po x 3 days; Tylenol or etc for pain. Then Acalabrutinib 100mg po 1X per day to monitor side effects. Should I wait to resolve this condition before restarting BTK Therapy with the Acalabrutinib???
ER visit after 13 days on Zanubrutinib (Diagno... - CLL Support
ER visit after 13 days on Zanubrutinib (Diagnosed 13yrs 8mos b4 needing treatment)
I developed pleurisy while in treatment on a clinical trial - it's very painful, sorry to say! There was no talk of stopping acalabrutinib. Why do you think you should stop BTKi treatment?
Zanubrutinib worked really good & quick but a bit too strong for me. My numbers are stable 4 days off Zanubrutinib. Hgb 10.8, Plts 59, WBC 56, ALC %95 #53. Platelets & WBC stay in the same range. Once I start I will be on it the rest of my life unless I do a Combination Therapy. One BTK incited this Lung Issue, I just figured I would clear it up before starting another. I want the greatest chance of success! I just met the criteria to start after 13yrs 8mos of no meds🙌🏾
I'm not sure of why you consider zanubrutinib caused your pleurisy. In my case it was probably because of opiods for extreme pain management and my limited ability to exercise, because I was spending most of the day on IV antibiotics for febrile neutropenia.
I take it you have just received the results of your latest blood test, because you noted a haemoglobin drop from 10.8 to 9.8 in your reply to Jammin_Me? You are still well above the threshold of 8.0 for a packed red blood cell transfusion, but you do need to ideally stay on zanubrutinib to maintain control of your CLL and keep working on the bone marrow infiltration, so that your platelets and haemoglobin recover.
With respect to your long period of watch and wait, remember that a third of us never need treatment. What do you know of your prognostic markers, in particular your CD38 expression from your flow cytometry test, FISH test results, LDH, B2M and most importantly your IGHV mutation status? Perhaps you can later try a combination therapy approach? If you have good markers, you might be able to again have around a decade or more of watch and wait, particularly given your focus on improving your health.
Neil
I was told here in this group to start while I was still strong & keep my options open. I know that it hits you so you need some reserves, if possible before you start. Zanubrutinib was the only thing different. I had a tight routine. Yes my RBC dropped 1 unit without holding my iron, how low would it be if I listened? Yeah I hear the doctors on the Webinar talk about that 30% without treatment. They say that because the average age is 70, if those statics are still correct. So they die from lifetime diseases not necessarily the CLL. I stayed intentionally ignorant of my diagnosis. What I do know is no del17p or TP53 & the IGHV is inconclusive for the 2nd time. A Combination down the line is something to consider but right now I just don’t want to end up in any ER🤷🏽♀️I may sound all big & bad but with medicine I am a proven lightweight.
Well I wish I had a doctor to follow me. The Oncologist didn’t speak to me when I called about a large hematoma 6 days on the new medication. I got labwork done thru my PMD. Hgb dropped 10.8-9.8 & the Onc PA suggested that I hold my iron supplements so they can see where I am losing blood from. I said okay when will I see the Onc & she said that she didn’t know if he had clinic hours this week or next. I explained that I have been Anemic all my life & with the CLL dropping my RBC/HCT, the BTK Dropping it too & I drop so low I pass out? She said no problem, you just go to the ER & get a Blood Transfusion. That’s not proper management, you don’t create an emergency 🤦🏽♀️ I have to stay with this doctor for 1 more visit then I am insisting on the switch to an older female Oncologist. I’m a Critical Care Nurse & This Double Visit to the ER, we not repeating that. On Day 6 I think they should of suggested reducing it so I could adjust better. But with Acalabrutinib the best tolerated, I am starting slow with a half dose. I don’t do well on meds, Natural Remedies work the best for me😍
CoachVera55, more power to you. Keep advocating for yourself! I have no desire for this watch & wait period I'm in(now 3 years) to be a time to watch my health deteriorate as a result of my CLL or my negligence to be informed of healthy practices. I'm 74 and have a lot of living to do! Many (not all) doctors today run their medical practice as a business 1st and are guided by insurance or the medical system they belong to. THEY ARE EMPLOYEES! Yuk! I hate seeing this. Search for a doctor that follows his intuition and his knowledge of who you are. They are out there treating their patients from their caring hearts. My previous caring oncologist went back to his home country. He was great! So far, after only3 visits, my new oncologist, though he rushes the 15 minutes of a scheduled appointment, has shown this same caring attitude. Time will tell. 🙂Sandra
Thank you & advocating is what I did for my patients over my 30yrs in the Nursing Fields. It doesn’t add to making administrative friends but it keeps the BS to a minimum. I am very afraid of the Broken Medical System & can no longer just cry about it. I will have to take formal steps because this is not ok! My 41yr old Onc is lazy & he is a professor. He may be a great teacher but a horrible bedside manner, he lies & contradicts himself. He even stomped out the room having a temper tantrum, not just not okay but very dangerous, smh 🤦🏽♀️ I pray you got a good one & I need 2 since Respiratory is a big part of my medical history & a new Onc. #GODSPEED
Yes I had a HomeCare Infusion Patient with a teenage daughter with Cystic Fibrosis. Yes they have special vest. And yes the Vibration Plate is recommended for draining the Lympathic System. We had beds in ICU that helped with Pulmonary Toileting & they function like the Vibration Plate… Its all good!
The difficulty you have is that you need to continue taking the drugs to clear your bone marrow which is at the moment infiltrated with CLL cells. If you stop, your CLL won't be restricted anymore and the infiltration will continue, this will be causing more issues and you will soon be dealing with something else. Only your doctor can make the call but sometimes you just have to push through for a while and it starts getting easier when your bone marrow is healthy enough to produce enough healthy cells again. It can take time, it can be scary and it can seem like being totally contraproductive as you don't seem to be getting better just worse - if I ever felt that way (and I certainly did) - I reminded myself that without starting treatment, I would have probably been dead already. You are not loosing blood anywhere, it is the drugs killing off you CLL cells and your body is not able to produce enough healthy cells yet, it isn't unusual for other blood counts to be affected when you start the drugs, your bone marrow isn't functioning well at this point.
I know it's scary but try to keep going, it will get better, trust me.
Its absolutely scary & I am starting the Acalabrutinib half dose. Ending up in the ER is not an acceptable result. My anxiety was on 10 with all the unmasked coughing patients & staff. I need the slow ramp up. Just need to know when to restart. I was in the ER & they ran all the basic & superb tests to rule out a heart attack but the Pleurisy was ignored & I suffered more unnecessary as my lung collapsed. So pardon me if I institute my old nursing knowledge of ABC & A is Airway which takes priority over the CLL right now. Hgb is up to baseline 10.8, Plts/wbc are both low & with the meds they were both high. I will start sooner than later. I just need to be able to exchange oxygen before the medication beats me up again. Its the beginning & I still have wiggle room.
Sorry CoachVera, it definitely needs dealing with first, you are right. I just wanted to point out that it's the CLL working in the background and wanted to encourage you to try to persevere with the CLL drugs as otherwise it becomes a bit of a vicious circle. I can totally relate and understand how upsetting and scary is to end up in the A&E, I was admitted to ICU with a neutropenic sepsis 10 days into my treatment and my instincts were telling me, surely I must stop taking these drugs if it's making me so sick...same two weeks later when my Hb dropped to 72...
All the best.
It is so scary that i am there holding my chest, in pain with an abnormal EKG. And the doctor is telling how my pulse ox is 98%. I have witnessed a patient tell the doctor that they can’t breathe while on oxygen. The doctor does nothing but assures the pt that he is fine, he leaves & the Patient Codes🤷🏽♀️
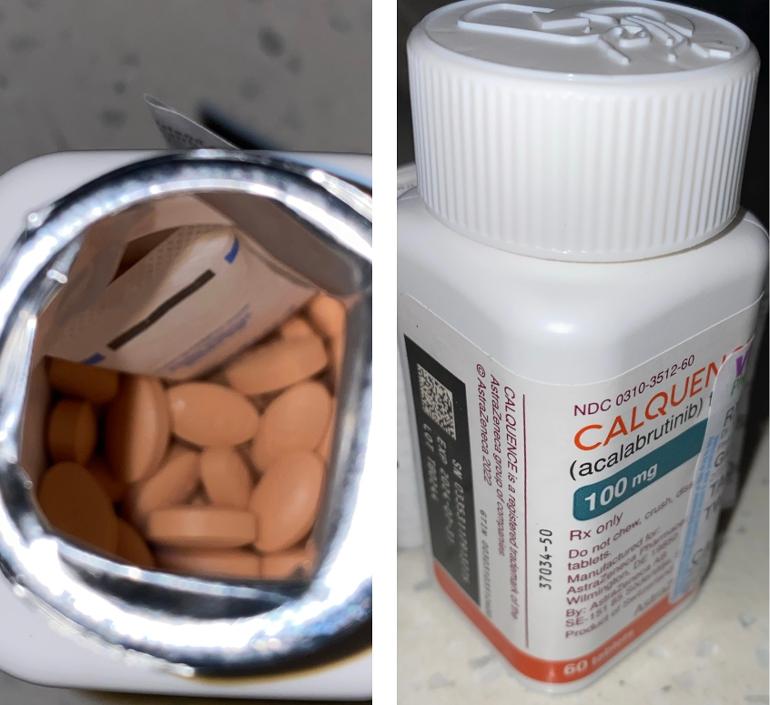
Nah I don’t want to mess up again, so I started the Acalabrutinib today 1 per 24hrs for a week. I did it there way with a bad outcome, now I will do it my way which is supported by the manufacturer insert. Error on the side of caution is what I have been told my entire 31yr RN Career & it works! Now I will work on finding a Pulmonologist because this ain’t over, it will try me again.
You need more rbcs and platelets. Your marrow is infiltrated with ccl cells and may be too crowded for normal hematopoesis.
If you tolerate the Acal I would go to the recommended dose of one every 12 hours and let it clear some space in your bone marrow for myeloid cell production.
I started it today, Acalabrutinib 100mg 1X per day & will monitor myself closely. I have 0 trust in them. What I need as an Asthmatic is to be able to breathe. I have Cardiac Arrested 3X & only GOD saved me, so that is who I trust. And my own 31yrs as an RN. What I needed was for the Left Pleural Effusion to be dealt with but its nice to have EKG/Echo/Heart Catscan to r/o PE & of course a CTA of my Coronary Arteries. All clear & clean with 0 calcium or plaque. But they were watching my lungs collapse- never again.
I am sorry you are having such pain. I am not liking the response of your oncologist at all. If it were me, I would look for a CLL specialist immediately and a pulmonologist who are willing to work together.
I didn’t see in your explanation what caused the pleurisy.
In any case, I hope you begin to feel better soon.
Yes this could be seen as a self fulfilling prophecy but I think its my clairvoyance. I came in strong & felt reduced to a germ in a petry dish just holding my heart & moaning with no help whatsoever. They were excellent in the SIUH Northwell ER ruling out a heart attack but made no moves to resolve the pulmonary issues. Its so disappointing & raises my anxiety to an unbearable level.
I have a Critical Care Referral for a Pulmonologist associated with my Cardiologist & Oncologist but only problem is they have no emergency appointments, can’t be seen until July 3 & I am still having the problem now May 10. Just not safe practice for me 😩
Oh Pleurisy started after my 2nd day of returning to my workouts, I clearly overdid it. I started Zanubrutinib full dose 2 pills every 12hrs on April 24. I canceled my 1hr Low Impact Class that I taught 2X per week that Monday but Thursday (72hrs on Zanu) I taught it with no issues. The fatigue & other side effects started kicking in & I did not teach for a week; Mouth Sores, Caustic Stool irritating my hemorrhoids, sore feet & painful tingling of fingers Day 5. By Day 7 large dark hematoma which I reported to Oncology. Got labs thru PMD that showed Hgb 10.8-9.8, Plts/WBC 79-80s now 118/108. I was advised by Onc PA to stop my iron supplements to see if I was bleeding from the bladder/GI Tract/Subcutaneous or even a Brain Bleed Anna the PA suggested. Being anemic all my life I refused that methodology since she could not tell me when I’d be able to see the Onc MD. I said it doesn’t matter where the drop is coming from because we know whats causing it & modifying the medication was my recommendation & I wish I followed my own mind then.
I stayed full dose & very painful joints preceded & my solution to sitting/laying around was to exercise because it helps my head better than my body almost. Friday I did 45min on my Treadclimber & I was good. Saturday I tried the Stationary Bike for 60min & felt a chestpain on the cooldown part @7:30p. The pain lasted 3hrs with no change & my son got me to the ER. They gave me nothing for the pain but the benadryl & steroids required for my Contrast Dye Allergy must of reduced the pain. When the 9/10 pain Dropped to 3/10, I left Sunday Afternoon AMA.
I had Oncology that next day where we made the request to switch drugs. No one cared about my Respiratory Distress/Chestpain, just about continuing the Zanubrutinib. By Tuesday I seen my Pulmonologist of almost 30yrs & he just watched my lung collapse saying he could do nothing. I reminded him how he treated me with steroids & antibiotics in the past but he was adamant about not helping me so off to the ER again but by Ambulance this time. All the while my son is helplessly watching me deteriorate in his face. It was awful. I had to beg for Morphine to rest for the CTA of my Coronary the next morning but with the Nitroglycerin & Steroids I was good again for awhile. I begged for steroids to go home & as the IV steroids wore off I felt a ROCK in my chest again that I could not breathe pass. I broke out the antibiotics & Nebulizer. Pain is worst laying down but I don’t feel full inflation of my left lung that showed further expansion of Left Pleura Effusion rule out Atelectasis VS Pneumonia 🤷🏽♀️ This sucks😩
When I had a pleural effusion (which is different from pleurisy), I definitely noticed that laying flat made my shoulder hurt. I slept in a recliner chair for six weeks until it cleared. I was fortunate (in a way) that I knew what caused the pleural effusion - I had broken a rib which punctured my lung.
It has to be horrible to not know why this is happening.
Now that is interesting, I have a history of Costochondritis & also of Unstable Angina. Once the heart was ruled out one ER PA suggested it could be Costochondritis but no one treated it. In the past it was Steroids/NSAIDS/Antibiotics/Pain Meds but somehow since Covid, my Pulmonologist is meaner. I don’t know why but I do know I need a new one because my lungs literally collapsed in his office & he did nothing but debate with us. Oh I also have bad osteoarthritis of my left shoulder, left rib & left hip.
IMO the excessive exercise during induction is aggravating if not contributing to this. It's not just a slow ramp up you may need, please consider Stop Doing All This Extra Exercise. I've written before how some of us need to be "hospitalized at home". If we feel fine and don't have symptoms, that's one thing. But to extremely push yourself physically when your body is already expending a tremendous amount of energy killing & metabolizing & excreting CLL cells seems counterproductive. You can force yourself to move skeletal muscle, until other organs say "stop it's too much" and they stop working optimally. I get the desire to exercise, but *meditation* exercises, stretching, yoga, will probably help more early into induction if you are having physical symptoms of dealing with CLL die-off. Pleural effusions and other lung things can happen as we are killing off these lymphoma cells, our lymph nodes are already pumping hard, and IMO if we push ourselves too much physically additional problems can occur. Docs tell us to "go about our normal activities" but the average person does not do hard physical exercise while under treatment. When people are treating an infection or having another illness, one *rests* a bit more. That's a SOP in medicine, let your body heal. We don't have to be bedridden like standard chemotherapy protocols, but that doesn't mean it's OK to push ourselves to do stuff any more than it would if our diagnosis was pneumonia or a UTI. Please consider things like meditation, and resting a bit more, instead of hard exercise, during induction. It may not be "the drug", it's "the drug with all this hard exercise."
I would have to agree & ‘hard’ exercise was my major coping mechanism. I am flying right from here on. I imagine its not a walk in the park & I just hope I can handle it. I will do anything to not end up in another ER. Now I just need sound advise while I go easy. Should I start back with Acalabrutinib just every 24hrs to see how I do or restart full dose every 12hrs since its ‘more tolerable & less effective’ than Zanubrutinib?
With multiple medical problems, the docs need to be the ones to say what & when. Your symptoms & labwork should dictate how you move forward, not advice from people who aren't doctors and don't have your medical records. None of us know the severity of your other disease states, and how those/any meds for them, may affect your CLL or any lab tests. The docs need to decide the order of things IMO.
If anyone here has had the exact same problems, they can relate what *their* doc did. But once comorbidities and unusual side effects during induction start cropping up, it's back to the docs. I am comfortable discussing what I think a doc might do, given what I have seen them do in the past, and what the literature recommends, for treating CLL alone with basic, common problems. When it starts getting complicated....no. Other than, the recommendation is to give one BTK a fair trial before deciding you need to switch, barring something super severe.
Yes of course but telling me to stay full dose on a new medication while still having chestpain (literally watching me holding & massaging my chest) & totally dismissing the Pulmonary Findings ‘Bibasilar Subsegmental & Dependent Atelectasis’(5/7). Even asking am I sure its not epigastric on 5/8 at in person visit. 5/9 I get to my Pulmonologist who does nothing but watch me go into extreme respiratory distress & back to ER by Ambulance since I can not breathe at all.
CTAngio Heart & Coronaries w/IV Contrast 5/10 shows ‘Small Left Pleural Effusion with adjacent consolidative opacities may reflect Atelectasis vs Pneumonia’ I was discharged with 40mg of Prednisone for 6 days. Airway is the ABC of care, if you can’t breathe, your dead but no one focused on that. The earliest Critical Pulmonary Appt from the ER is July 3. So I don’t know which doctor would or could follow me. Next Onc appt May 31 but I started my Acalabrutinib today 100mg for 24hrs while I humbly monitor myself🤦🏽♀️
Oh I am an Asthmatic who Cardiac Arrested 3X as a child with multiple drug allergies. My Mom took DES while pregnant with me & my Grandfather was an unauthorized participant in The legendary Tuskegee Experiment
What does your oncologist say? Lymphomas can cause pleural space problems when treatment commences, including pleural effusion. Some oncs treat through an effusion, some don't. It's up to the doc. It's unlikely you will get BTK resistance holding for even a few weeks, some here have had to hold for surgery or drop in neuts/platelets.
My Oncologist says many different things & contradicts himself. He’s 41 & appears lazy to me. He said my doctor didn’t send my medical records. To that I said, yes she did, I made sure & confirmed it with your staff. I demanded that he opens his computer & there it was. He literally lied to me 4 times when I first met him. I can’t say that he is incompetent but I can see that he lacks integrity. I am a seasoned Critical Nurse & we don’t mesh right for this serious journey. Dr Dai is who I am switching to, she has 40yrs in this field, good reviews/testimonies & credentials. I have my eye on a specialist too but she is changing hospitals, I hear that she’s coming to Robert Wood Johnson where I worked & was diagnosed in 2009 & had my Bilateral Knee Replacements. So I may travel to see her. I have Cardiac Arrested 3X from Asthma so my Lungs are weakest link… I took 1 today & will do it for a week. I am on the hunt for a Pulmonologist now before 2 months. I will be in contact with pharmacy, we have a repoir. I have to conserve my energy with nonsensical stuff.
IMO you really need a full on CLL Specialist input on this, now that you are having complications. Or a hem-onc who is experienced in the lung issues with lymphoma at a minimum, if not a full on CLL Specialist. CLL is rare, & unless a regular hem-onc is willing to put in some time reading upon the most current recommendations, and review literature for how the specialists deal with problems, one won't get great care. I am reminded of the hem-onc who was "the person who treats the CLL patients" at one large facility, arguing with me that my SE's couldn't possibly be the drug, when those same SE's were listed in the package insert. I do not know what their thought process was, but I wanted none of it. This person was so unlike my first hem-onc, who in retrospect obviously read up on current concepts, etc. in CLL.
Sounds like you have a similar situation, this doc "doesn't know what they don't know" about CLL, and doesn't seem interested in finding out. I hope you can get some decent help soon.
My childhood friend who is an RN near 40yrs said you need a seasoned clinician like yourself. I had them in the beginning but have to get a new Pulmonologist & Oncologist. The Bibasilar Subsegmental Atelectasis was discovered on 5/7 so why wasn’t it treated then. Or 5/8 in my Oncology office or 5/9 in my Pulmonologist office. I was mistreated & it could of cost me my life. What has happened to our Healthcare System. They simply said that I was not breathing deeply🤷🏽♀️Everyone walked around the elephant in the room. I am on the search & coming in hot 🥵
When I started treatment last November, I was not in dire shape but any intense exercise (like cycling up hills) exhausted me for days afterwards.
SofiaDeo had recommended to take it easy when starting treatment and I followed her advice. I am still limiting myself to one bike ride a week. I still make my goal of 750 active minutes a week but this comes mainly from hiking. I can modulate my exertion more easily hiking than riding up a hill.
Some days I don’t exercise at all. My ALC has dropped by 30 to 40% every four weeks and my other counts are all normal again or nearly so.
I can’t say that following her advice is the reason everything has gone smoothly so far but I think it is reasonable.
Given that it may take 6 to 8 weeks to recover from your lung issues, I would, if it were me, start taking your CLL meds again, ramping them up if that makes you feel more comfortable.
Having leaned hard on exercise through the Covid pandemic to keep me sane, I know it’s hard to back off that. I was forcefully reminded that I am still “coming back” when I visited Fort Collins. We used to live in Albuquerque and was used to breathing at 5000 feet. But no longer. Now we live at 200 feet elevation.
While my family happily hopped up stairs in Fort Collins, I was breathless at the top of the stairs. I could barely manage a one mile walk the next day.
This clarified to me that my strength has not returned. I still need to ramp up slowly.
** One more thought - doctors are under a lot of pressure to not prescribe opioids for pain due to the number of overdoses. I noticed a huge difference between my first knee replacement and second one six months later, and this was back in 2013.
Absolutely to slow down while starting this new medication is words of wisdom & I will abide now lol. I didn’t ask or put it together since relieving stress was my goal & this is so stressful dealing with the unknown & not feeling adequately supported when things pop up. Its life lifing so I am aware now that walking will be it for me & 5-15min intervals at most. Thank you all for your words of wisdom👏🏾👏🏾👏🏾
Cyclewonder is right about the challenges of getting access now to opiates for pain management, particularly for pain management. The CDC really tightened up on their recommendations in 2019 and have only partly backed off this year. Deaths from fentanyl in the US have increased alarmingly, but most of that is from recreational drug use, not when prescribed.
You should not be using any NSAIDs while you have low blood counts, particularly when you have low platelet counts and especially when you already seem to be losing iron. Doing so will put you at risk of further blood count suppression and importantly, higher risk of gastrointestinal bleeds. Use Tylenol/acetaminophen for pain relief.
Finally, there's been no head to head comparison of acalabrutinib and zanubrutinib, so we don't know which one is more effective. I would say that the deciding factors for their use are which is best tolerated and which is easiest for dose reduction. Zanubrutinib wins out for dose reduction, but relative tolerance varies with the individual. Theoretically, acalabrutinib is the cleaner drug, off target wise.
Neil
Yes I know the bleeding risk so I said no to mortrin & took the Tylenol. When the pain became severe again I demanded Morphine. MONA is what the protocol is for Chestpain; Morphine, Oxygen, Aspirin & Nitroglycerin. They do package Acalabrutinib as the milder & less effective between the two. I am scared to run the risk of now making my CLL more resistant so I started Acalabrutinib today (1 week off) as I prayed over it🙏🏾🙏🏾🙏🏾
Could you please provide more detail on "They do package Acalabrutinib as the milder & less effective between the two."? Who is they? This 2021 study from Sweden Comparative Analysis of BTK Inhibitors and Mechanisms Underlying Adverse Effects, shows that acalabrutinib has less off target effects than zanubrutinib as listed in table 2 - it's a cleaner drug as I mentioned earlier, so could be experienced as a "milder" drug. ncbi.nlm.nih.gov/pmc/articl... I'd be very interested to know from where the "less effective" description was derived.
As I said earlier, relative tolerance varies with the individual. This study noted that Zanubrutinib Demonstrates Efficacy and Safety in Acalabrutinib-Intolerant Patients with B-Cell Malignancies onclive.com/view/zanubrutin... so could appear milder for those that can't tolerate acalabrutinib, but I expect that the same might be found, probably more so, if patients not able to tolerate zanubrutinib switched to acalabrutinib. Both drugs are considerably more tolerable than ibrutinib and come with a significant adverse event risk advantage. Beigene was able to establish itself in the BTKi market through the support of an Australian CLL researcher, who helped them set up clinical trials. They are slightly undercutting the price of acalabrutinib to help them establish market share. I wouldn't think that would be necessary if Acalabrutinib was less effective. Importantly, they are both effective at managing CLL.
Neil
I could imagine that they are fixing things from I to A to now Z & they seem so pleased with Zanubrutinib. I wish I could of stayed on it but full dose out the gate was too much. The mouth inflammation was giving me anaphylaxis mindset. The regular exercise I donwas just the catalyst, I was headed this way sooner or later. I know it works because all the xrays in the ER said ‘no lymphadenopathy’ ??? Dr Sharp an associate of my Onc said that if my CLL took 13yrs 8mos to need treatment then it’s probably a mild form & I want to believe that. I also have low tolerance to medications period. I have multiple job related injuries & surgeries & can not tolerate pain meds, any one of them make me nauseous & too loopy too long.
Thanks, so to quote from the information you were given, "When settling among the BTK inhibitors, we prefer acalabrutinib or zanubrutinib rather than ibrutinib. While we have the most experience and longest followup with ibrutinib, extrapolation of data from the relapsed setting suggests that acalabrutinib and zanubrutinib are at least as effective and better tolerated than ibrutinib. If the goal is best efficacy with acceptable tolerability, we offer zanubrutinib, in contrast if the goal is best tolerability with good efficacy, we prefer acalabrutinib." (with my emphasis. Zanubrutinib hasn't been trialled for long, so I'm not sure )
Isn't it good that we have three choices and growing! It will be interesting to see how that expressed preference pans out over time, because we don't have much long term data. Zanubrutinib was first trialled in 91 participants with CLL in China in 2017 and then commencing in May 2020 in Australia with 150 participants with follicular lymphoma and CLL, There are plenty of trials happening now!
As I noted before, with your long watch and wait, if you can convert to a fixed term combination treatment, you should be able to expect a long remission. A big advantage of these targeted therapies, is that unlike the older chemoimmunotherapies, they don't cause DNA damage to the CLL (which could potentially causing harder to treat sub-clones as we saw with chemoimmunotherapy) or to any other body cells. That means that provided resistance doesn't develop, you should be able to repeat the combination treatment, though by then who knows what will be available?
Neil
Hi Neil, side question. I'm stage zero, del 13q, my CLL specialist mentioned that my CLL itself has its own mutation but didn't seem worried about that. Should I press?
I'm assuming the mutation your CLL specialist mentioned is your del 13q (part of the longer arm of chromosome 13 is missing), but you might like to verify that's what they meant. 13q del is actually the most favourable FISH result you can have - even better than having no mutation reported from the DNA probing done.
Neil
Yes, that is the deletion, but then there is a mutation within the cell itself called a dicer1 gene mutation. Dr. Patel said it was "unusual" but did not mention it might indicate any additional difficulties in treating if and when that time comes. But I did not think to ask. I am thinking now that I should press him on what that dicer1 might mean in potential treatment. Have you ever heard if it?
Here's some info on DICER1. Not sure how it may contribute to CLL per se. It has been associated with other tumors. Not everyone who has a DICER1 mutation develops problems associated with the mutation. Since you have reached adulthood without getting a "DICER1 syndrome" diagnosis, your other one probably works well enough.
Just looking at the drugs listed you could see that Zanubrutinib is the second strongest after Ibrutinib by the size of the dots. I felt it come in heavy. But what I believe I am seeing is how they designed them. As the trials go on over time that is where they have tweaked things. Imagine 13yrs 8mos 0 treatment & then after 13 days of treatment it attacks my lungs. With all this inflammation from the CLL, my chest & abdomen are out of whack. My whole body got hit with a Mack Truck. I pray this Acalabrutinib will do the job & be gentle lol🙏🏾 I still got to heal but I started Friday. 1 week off & now we will ramp up & go by my symptoms. I need a good Pulmonologist for this to be successful 🙌🏾
The ideal inhibitor drug would have just one large red dot for the BTK in CLL cells - and no other dots. The size of the dots elsewhere shows the degree of the off target effects for kinase inhibitors in other body cells. If you have a closer look at the plots for acalabrutinib and zanubrutinib, you'll see that there are similarly large dots on both the acalabrutinib and zanubrutinib plots for the BTK in CLL cells, but acalabrutinib has less dots and those are smaller than those for the other BTKis. As I said, acalabrutinib is a cleaner BTKi. However, zanubrutinib is easier to dose reduce.
Neil
What I remember most about the question I posed about starting treatment was someone said after 2 weeks they put CLL in the rearview mirror & went on with their life & that is exactly what I want🙌🏾
I shut down the Fitness Classes until further notice. I dropped the whole CDC NDPP Program when I hit stage 4, Oct 2022. I know that CLL has a better prognosis than solid tumors but it takes its toll on you too. I look forward to it working & once its manageable then I can go live my life Abundantly. So yes that will be exciting 🎉
There is no "stronger" or "strongest" when comparing different drugs, even within the same class. There are *differences* and *different effect/side effects*. And then one has to see how that translates to actual people, and how differences in various patients (age, sex, race, comorbitidities, GI function, diet, whatever) happen to affect anything. You are reading the chart incorrectly. It is not a measure of "one is stronger than another" it is a description of the type and amount of certain effects. In real life, one will "work better" with "fewer side effects" depending on the patient. You were critical care, correct? Recall how some people varied in their response to different antihypertensives of the same class. You start with one, if it doesn't give the desired effect with minimal SE's, you move on to the next. So if an ACE inhibitor was recommended, and the first one wasn't working well, one switched. But one never spoke of one ACE inhibitor being "stronger" than another.
I would have to disagree altho I love you & your input❤️
Lets look at a Diuretic, I am on HCTZ 25mg 1X per day for Blood Pressure. It is mild & is supposedly Potassium Sparing. So when we medically remove fluids, potassium leaves too. So if you need mild removal go with HCTZ but if you need more, than Lasix & one of the strongest is Bumex. You will need to check your labs frequently until we establish your baseline on the latter two. So yes based on your medical condition & purpose, plus you should always start low & move up if not in an emergency situation.
I got Morphine during my twins birth via my spinal cord with an epidural & had a horrible urticaria reaction (itching). Because it bypassed the digestion system it raised the possibility of a reaction. I have it now with Benedryl when needed for chestpain.
But the graph is showing where there are rates of inhibition. I see Zanubrutinib as the 2nd highest of massive on target 100% Inhibition next to the original Ibrutinib. The others have lower inhibition but more on target. I am 2 days on Acalabrutinib & I felt finger tingling & now headache. Another supporter suggested side effect remedies in place to increase tolerance. What do you think about data of side effects & treating the side effects during treatment as opposed to needing an ER visit?
You forget these numbers are based on lab tests. There is no guarantee that you will have fewer effects with one over the other. It's a list of effects based on current tests. A likelihood of SE's, but not absolute. Especially in drugs that have only been out a few years, used in a rare disease. There isn't enough experience t note any statistically significant in vivo differences from the lab test.
Re the "stronger" versus "weaker", "milder", you may choose to use those terms colloquially, but they are not used in the literature. We talk about drug comparisons in terms of "mg strength", potency, and effectiveness. So in your hypertensive scenario, the treatment algorithm calls for starting with a low potency agent, then proceed up the chain as the desired effects are not reached. Bumex is the most potent, and loop diuretics generally are, which is why a thiazide like HCTZ is used initially. The drugs themselves aren't inherently "stronger" or "weaker" overall, especially when talking about different mechanisms of action. In many diseases the selection and dosage of drugs depend on the degree to which one or more particular factors are present. It has more to do with disease presentation and associated things, than any overall "strength" of the drugs under consideration. IMO anyway haha  I guess if you spoke in terms like "I think, looking at the data, zanu might have been a better initial choice for me" or "based on X and Y I would like to switch" I wouldn't be pointing this out, because I think it's not because one is inherently "stronger" than the other.
I guess if you spoke in terms like "I think, looking at the data, zanu might have been a better initial choice for me" or "based on X and Y I would like to switch" I wouldn't be pointing this out, because I think it's not because one is inherently "stronger" than the other.
Also note that the chart is not "in vivo" testing. Kinome profile is not numbers of measurements taken from actual humans. It's accurate, but a guesstimate, because once the drug is in the body it also interacts with other things.
I do understand your valid technical points on data collection, drug interactions & outside factors but I just see it in this simplified way 😂. I am a more broad stroke type of person because my first instincts are usually right 9/10 times.
Let me give you some personal data. I started the Acalabrutinib yesterday 100mg every 24hrs (1/2 dose & many stay here) & I am feeling that same left pleural effusion pain now. I had a whole 24hrs with no pain. My fear is that the Acalabrutinib is affecting my weakest links, so do I fight thru it or stop again🤦🏽♀️. I am following Dr Goggle with the Pleurisy treatment of steroids, antibiotics, Neb Tx & Tylenol (until I can find a Pulm). Its not pain per se but I feel rattling in that same spot. I will breathe deep, hydrate & pray it lives. I will even sleep in my lounge chair. Another ER Visit is not on the agenda😫 Oh BTW I felt the finger tingling yesteday & Bilateral Knee Pain today. What is a lighter more gentle treatment with minimal side effects out there for CLL???
Since lymphoma treatment (CLL is a lymphoma) can induce pleural effusions, if I were still working oncology & you were my patient, I would have suggested to the team that any restart be done on a Mon or Tues, so any continued pleural effusions could be monitored. Since you have started some sort of a lung process, induced by some combo of all the exercise, on top of the med, and a history of lung problems. If you are having a pleural effusion, it may not be something that you can "fight through" alone. I know it's a hassle on a minor holiday Sunday, but if you are having labored breathing, lung filling up, it may be wise to get seen. If you truly are having an effusion, you know at a minimum you likely need a diuretic. It's unclear to me what about your CLL makes it necessary to restart given your unresolved lung problems , but I am not a lymphoma specialist.
Side effects/adverse effects/ unexpectedly rapid cancer cell die off, are some reasons I recommend starting new drugs on a Mon or Tues. On all the cancer teams I worked with, this was SOP. Even on some non cancer teams; a rheumatoid arthritis patient starting *methotrexate* was asked by the clinic to wait until Mon or Tues to start, in the event the patient was extremely sensitive to anti platelet effects. I guess I have worked at some really good places, hearing some of the issues some of you have had.
Please remember, just because these are pills instead of us being hospitalized hooked up to IV's 24/7, doesn't mean side effects needing treatment are not a possibility. People can unexpectedly have a rapid response, or cell lines drop precipitously within the first 48-72 hours. Pleural effusions, although rare, can occur with lymphoma treatment including CLL. It's great we can more or less "go about our normal lives" but excessive hard exercise, and trying to wait out a symptom as if this were a minor cold, may not be a good idea.
Yes starting on a weekday is excellent advise. I am an Asthmatic since 18mos old. I cardiac arrested 3X under my Mom’s care because she listens 100% to doctors. I know how to toilet the lungs & I got alot of practice with the AIDS Patients. I have the Steroids, Antibiotics, Nebulizer, Tylenol & trust in my LORD. If I don’t panic I can make it. I think the BTK Inhibitor is causing the movement of this ‘exudate’ & it will definitely have me resting & deep breathing for this entire induction period (how long is that?). I do have my HCTZ that I take earlier now & I am mostly clear with crackles at the left base. There is a pocket of fluid that I can feel with each inspiration & expiration. Its not rubbing because thats what the pain was caused by. I just need to stay hydrated too. Lung PT is what is necessary & what I’ve done for decades, I got this. I need a Pulmonologist Oncologist, CLL Specialist (or just have a conscious) & also a Lawyer.
The Doctors; On 5/7 ER Cardiology called (never met him) to say that after speaking with my Oncologist & Cardiologist they all held the stance of continuing the BTK (not sure why, no rationale given). My Oncologist told me in his office on 5/8 while I held my chest to minimize the pain that Zanubrutinib doesn’t have chest pain listed as a side effect. He also asked me if I thought the pain might be epigastric? He did not offer any rationale why to continue. He went on to say that he did not know if my insurance would make the switch to Acalabrutinib. I had had enough of the insensitive discussion about the drug, no attention placed on me in pain in front of him & I told him (when able to produce enough oxygen to speak) to not worry about my insurance because the Pharmacist Samantha got it all handled. He gave me this sadistical smurk & I wandered out holding my heart & calling my old Pulm office & Cardiology office for a Walk In Appt. It was hell but I will have an opportunity to bring it back🙋🏽♀️
I do so appreciate all the brain power you are bringing to our discussions, thank you sincerely. What you might consider a ‘self fulfilling prophecy’ can also be, me knowing myself. So by restarting the BTK, I am following my Onc orders (altho half dose) & my rationale is when you stop abruptly things get shooked up. And when things start mixing & touching then an unforseen outcome can occur which only in hindsight you realize. I have seen some bizarre things in Nursing & Scleroderma plus Flesh Eating Disease is two. I have been Favored on this journey & I don’t want to mess it up more than I have already, so I made a decision & must follow it thru. Plus my Plts were scary low after stopping Zanubrutinib.(B4) 4/17 Plts 80’s (During) 5/2 Plts 118 (after) 5/7 Plts 40. I won’t do anything strenuous because Pulmonary Toileting is strenous for me right now🤷🏽♀️ I learn my lessons hard & rarely make the same mistake twice. I want CLL in my rearview so I will slowly ramp it up & I hope that doesn’t upset my perfect balance of proteins.
Much is still being learnt & I want to error on the side of caution. 3rd dose of Acalabrutinib in with only slight headache & fatigue noted today. To see my large framed 250lb self, it’s unbelievable to know how light weight I am when it comes to drugs but this is why I’ll do Natural Remedies All Day with 0 Side Effect & Strictly On Target Results👍🏾 I know GOD made medicine too & I blessed my bottle🙏🏾
I think it's more "any CLL treatment when someone has lymph nodes in the chest" can cause pleural effusion, not the BTK specifically. I have spoken with another who chose to do a lot of exercise early into V&O, and also got a pleural effusion. That person's CLL Specialist stated that lymphomas like CLL can cause pleural effusion. The literature states some forms of disease present with these effusions before treatment, as a symptom pre as well as after diagnosis. It seems reasonable that anything involving the chest nodes moving/changing rapidly may contribute to, if not cause, this process.
Thanks that is a good idea. I know the doctors are burnt out but I need someone to make it all make sense🤦🏽♀️
Yes I am glad that we have 3 BTK choices but honestly I am still going down this road kicking & screaming 🤦🏽♀️ Surviving the ramp up over 3 months & finding a new Onc & Pulm then I can get excited too. That 13 day usage ending up in the ER was my worst case scenario. So I can’t even see a combination therapy with toxicities doen the road. I have 13yrs 8mos of nothing & no ER Visits, so none of this is exciting to me. I still don’t know the extent of this damage. I have Cardiac Arrested 3X as a Child, Covid almost killed me 2yrs ago & all of this trauma now is getting to be too much🙌🏾
Sorry, but it does get easier.
I was completely unguided & mismanaged. I am still in shock. Chestpain started 5/6 @7:30 after 6omin on the bike. 3hrs later I call my son & off to the ER. Chestpain, abn EKG, placed in telemetry & on the monitor 1hr later. Chest Xray, Bloodwork/troponin & IV. Catscan r/o PE, then Echo. By 5/7 we know Bibasilar Subsegmental and dependent atelectasis but no treatment. Multiple doctors, Cardiology, ER PA, My Onc, My Pulmonologist (28yrs) all said I am not taking deep breaths. This mess progressed to a Collapse Lung. I went into Respiratory Distress in Pulmonologist Office & he offered me no help.
My Medical History includes Cardiac Arrest X3 from Asthma. So I don’t have much reserve here. I am still in shock, just wow 😮 So I will manage this until I get a real Oncologist & Pulmonologist. Then it will be tight & right🙌🏾
CoachVera, you've had a tough time and your post makes for uncomfortable reading. I like your last two sentences and really hope that's how it works out. Best wishes.
It was scary but we all need to be forwarned & forearmed. Minimizing the effects of this strong drug caught me off guard, don’t be fearful but be cautious if its new to you or like me who don’t do drugs. My system is virginal & I need a lighter dose & closer monitoring. I was taught to error on the side of caution, people don’t die when you are extra cautious. We are all different with different levels of tolerance. We are so blessed to be able to have all these choices; longterm treatment or combination short term therapy. Always report your side effects & ask for their plan of treating it, stay on the same page with your Onc team. GODBLESS Us All🙏🏾🙏🏾🙏🏾