After surgery and salvage radiation therapy (SRT) have failed, it appears I'm headed for androgen deprivation therapy. Like many things in the world of prostate cancer, the recommendations as to when to start ADT seem to be all over the place, so I'm seeking any insights folks may have based on your own experiences.
Background
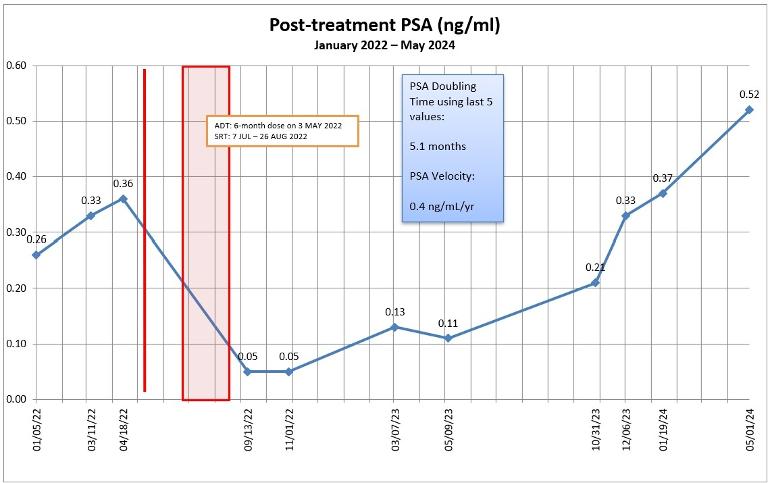
Nov 2010 — Diagnosed at age 52. Routine physical exam revealed palpable mass during DRE. PSA 5.0. Biopsy revealed Gleason 3 + 3.
Jan 2011 — Radical prostatectomy. No seminal vesical or lymph node involvement; no extra capsular extension; negative margins; pathological Gleason 3 + 4.
Sep 2015 — PSA went from undetectable (<0.03 ng/mL using this lab) to 0.05 ng/mL. PSA bounced around between 0.04 and 0.08 for about 18 months.
Jul 2021 — PSA hit 0.21, passing the traditional definition of biochemical recurrence of 0.20.
Nov 2021 — PSMA PET scan at PSA 0.23 ng/mL; negative for prostate cancer.
May 2022 — Received six-month dose of Eligard in advance of SRT. PSA 0.36 ng/mL.
Jul – Aug 2022 — 35 sessions of SRT to prostate bed only; 70 Gy.
Nov 2022 — PSA 0.05, mainly from effects of Eligard.
Mar and May 2023 — PSA 0.13 and 0.11 respectively.
Oct and Dec 2023 — PSA 0.33, 0.37, respectively.
Jan 2024 — PSMA PET scan at 0.37 ng/mL; negative for prostate cancer or metastases.
May 2024 — PSA 0.52; PSA doubling time dropped to 5 months.
What's Next
In February, I met with a medical oncologist for the first time (when my PSA was 0.37 and just had a negative PSMA PET scan). In a nutshell, her thoughts were to wait about 6 months (August 2024) and see what happens with the PSA and to repeat a PSMA PET scan to see if we could determine what was really going on. If the scan revealed lesions, then we might be able to go back and zap them with additional radiation therapy.
She was also inclined to delay the start of ADT until my PSA hit 2.0 ng/mL, and she was thinking it would be just ADT and not a combination therapy with an antiandrogen. We really didn't get into the discussion as to whether it would be continuous or intermittent ADT.
Research
Here are three research papers that I've come across addressing this topic.
ncbi.nlm.nih.gov/pmc/articl...
ncbi.nlm.nih.gov/pmc/articl...
ncbi.nlm.nih.gov/pmc/articl...
I'm going to reread them, but my general take-away was that there wasn't a general consensus on the timing or the benefits of early ADT.
Questions
I have an appointment with my urologist on 14 May 2024, and I'm sure we'll discuss this in detail then. For the group:
▫ Does starting ADT early delay metastasis?
▫ If ADT is started early, will that make the cancer ADT resistant earlier?
▫ Aside from not experiencing the ADT side effects, is there an advantage to delaying the start of ADT?
▫ Is there a PSA threshold at which ADT should be started?
▫ Is there a PSA doubling time threshold at which ADT should be started?
▫ Any advantages to continuous vs. intermittent ADT?
(Yes, I realize that every case is unique and that very few of us in these forums are medical professionals. I just value insights gained from others' experiences.)
Summary
While I tolerated the six-month dose of Eligard pretty well, I'm in no rush to start ADT. My inclination right now is to wait 2-3 months and get one more PSMA PET scan done to see if it can finally reveal what we're dealing with before starting any further treatments, whether it be more radiation therapy or starting ADT.
If you've made it this far, thanks!