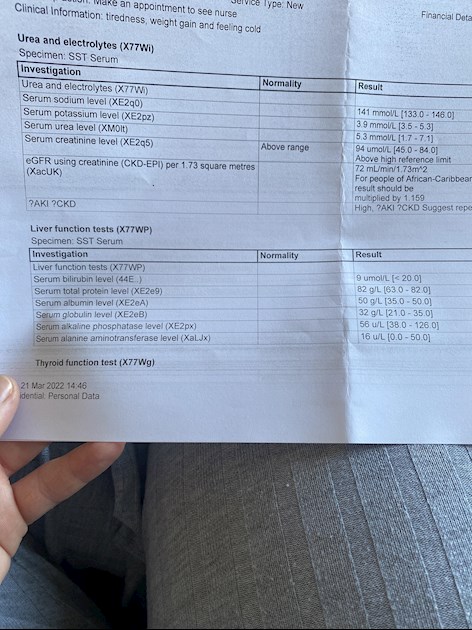
I have no idea what any of this means but I have finally got my results from the doctors, this is my first one back in December and will post my one from March too
Blood tests results : I have no idea what any of... - Thyroid UK
Blood tests results
Related post with latest results here:
healthunlocked.com/user/han...
Emmajane1994
There are no thyroid function tests on that sheet. Is there only one sheet from December? "Thyroid Function Test" is showing at the bottom so there should be a second sheet.
Your March blood test in your other post shows your TSH to be 4.14 (0.35-4.94) which is now in range but it is too high. The aim of a treated hypo patient on Levo only, generally, is for TSH to be 1 or below with FT4 and FT3 in the upper part of their reference ranges, so this is ultimately where you may feel best.
Your GP may say your TSH is now fine because it's in range but although useful for diagnosis once on thyroid hormone replacement it's the FT4 and, more importantly, FT3 results that tell us our thyroid status.
You need an increase in your Levo - 25mcg now and retest in 6-8 weeks. Ask your GP for this increase and to support your request use the following information if he is reluctant to increase your dose:
From GP online
gponline.com/endocrinology-...
Under the section
Cardiovascular changes in hypothyroidism
Replacement therapy with levothyroxine should be initiated in all patients to achieve a TSH level of 0.5-2.0pmol/L.
Also, Dr Toft, past president of the British Thyroid Association and leading endocrinologist, states in Pulse Magazine (the professional publication for doctors):
"The appropriate dose of levothyroxine is that which restores euthyroidism and serum TSH to the lower part of the reference range - 0.2-0.5mU/l. In this case, free thyroxine is likely to be in the upper part of its reference range or even slightly elevated – 18-22pmol/l. Most patients will feel well in that circumstance. But some need a higher dose of levothyroxine to suppress serum TSH and then the serum-free T4 concentration will be elevated at around 24-28pmol/l. This 'exogenous subclinical hyperthyroidism' is not dangerous as long as serum T3 is unequivocally normal – that is, serum total around T3 1.7nmol/l (reference range 1.0-2.2nmol/l).*"
*He confirmed, during a talk he gave to The Thyroid Trust, that this applies to Free T3 as well as Total T3 and this is when on Levo only. You can hear this at 1 hour 19 mins to 1 hour 21 minutes in this video of that talk youtu.be/HYhYAVyKzhw
You can obtain a copy of this article from ThyroidUK:
tukadmin@thyroiduk.org
print it and highlight Question 6 to show your GP.
Ferritin: 35 (23-300)
This is low. Ferritin is recommended to be half way through range and some experts say that the ideal level for thyroid function is 90-110ug/L.
Below 30ug/L is considered iron deficiency by NICE so you can see how low yours is.
I would suggest asking your GP to do an iron panel consisting of Serum Iron, Transferrin Saturation Percentage, Total Iron Binding Capacity and Ferritin. This will show if you have iron deficiency. Also ask for a full blood count to see if you have anaemia. You can have iron deficiency with or without anaemia.
With such a low ferritin level your GP may offer iron tablets so take these with Vit C to aid absorption and take iron 4 hours away from thyroid meds as it will affect it's absorption otherwise.
If your serum iron and the other tests are fine and don't suggest iron deficiency or anaemia then you can try and increase your ferritin level through diet. You can help raise your level by eating liver regularly, maximum 200g per week due to it's high Vit A content, also liver pate, black pudding, and including lots of iron rich foods in your diet
bda.uk.com/resource/iron-ri...
everydayhealth.com/pictures...
Your liver function tests and Us and Es are all within range and seem fine.
Vit D: 31nmol/L
This is very close to deficiency (deficiency is <25 in some areas, <30 in other areas.
What is your GP doing about this, if anything? You really need something close to the loading doses plus D3's important cofactors. If you come back and say what your GP is going to do I'll let you know if the dose of D3 is enough.
Folate: 5.9 (2.7-15)
Folate is recommended to be at least half way through range so that would be 9 plus with that range. Eating folate rich foods and taking a good quality B Complex will help raise your level.
B12 - We don't normally see a holotranscobalamin test result, usually just a Total B12 result so I'm not sure what Total B12 <300 reflexed for HoloTC means other than perhaps your result was less than 300 for Total B12 so they automatically do the other test to rule out B12 deficiency. It's a shame you haven't got the Total B12 result because that would determine whether or not you need to take a sublingual B12 as well as a B Complex.
For B Complex I have used Thorne Basic B for a long time and always been happy.
If you look at different brands then look for the words "bioavailable" or "bioactive" and ensure they contain methylcobalamin (not cyanocobalamin) and methylfolate (not folic acid). Avoid any that contain Vit C as this stops the body from using the B12. Vit C and B12 need to be taken 2 hours apart.
When taking a B Complex we should leave this off for 3-7 days before any blood test because it contains biotin and this gives false results when biotin is used in the testing procedure (which most labs do).
Emmajane1994
By the way, your last two images are showing your name and national insurance number. This leaves you at risk of identity theft, you may wish to remove the images and resubmit without those details showing.
My results were apparently all fine.Just a little low in vit d and to get in the sun when it comes out 😂 no medication was given to me
Even if your area defines Vit D deficiency as <25 then your level of 31 comes into the "inadequate" or "insufficient" category and requires addressing, some doctors will prescribe a low dose D3 at this level but some just advise the patient to buy their own which in most cases is the better option.
Not everyone can make Vit D from the sun.
The Vit D Society and Grassroots Health recommend a level of 100-150nmol/L, with a recent blog post on Grassroots Health mentioning a study which recommends over 125nmol/L.
To reach the recommended level from your current level, you could supplement with 5,000iu D3 daily.
Important to retest after 3 months.
Once you've reached the recommended level then a maintenance dose will be needed to keep it there, which may be 2000iu daily, maybe more or less, maybe less in summer than winter, it's trial and error so it's recommended to retest once or twice a year to keep within the recommended range. This can be done with a private fingerprick blood spot test with an NHS lab which offers this test to the general public:
Doctors don't know, because they're not taught much about nutrients, but there are important cofactors needed when taking D3. You will have to buy these yourself.
D3 aids absorption of calcium from food and Vit K2-MK7 directs the calcium to bones and teeth where it is needed and away from arteries and soft tissues where it can be deposited and cause problems such as hardening of the arteries, kidney stones, etc. 90-100mcg K2-MK7 is enough for up to 10,000iu D3.
D3 and K2 are fat soluble so should be taken with the fattiest meal of the day, D3 four hours away from thyroid meds if taking D3 as tablets/capsules/softgels, no necessity if using an oral spray.
For D3 I like Doctor's Best D3 softgels, they are an oil based very small softgel which contains just two ingredients - D3 and extra virgin olive oil, a good quality, nice clean supplement which is budget friendly. Some people like BetterYou oral spray but this contains a lot of excipients and works out more expensive.
For Vit K2-MK7 I like Vitabay or Vegavero brands which contain the correct form of K2-MK7 - the "All Trans" form rather than the "Cis" form. The All Trans form is the bioactive form, a bit like methylfolate is the bioactive form of folic acid.
If looking for a combined D3/K2 supplement, this one has 3,000iu D3 and 50mcg K2-MK7. The company has told me the K2-MK7 is the Trans form
natureprovides.com/collecti...
It may also be available on Amazon
Magnesium helps D3 to work. We need magnesium so that the body utilises D3, it's required to convert Vit D into it's active form, and large doses of D3 can induce depletion of magnesium. So it's important we ensure we take magnesium when supplementing with D3.
Magnesium comes in different forms, check to see which would suit you best and as it's calming it's best taken in the evening, four hours away from thyroid meds if taking magnesium as tablets/capsules, no necessity if using topical forms of magnesium.
naturalnews.com/046401_magn...
drjockers.com/best-magnesiu...
Don't start all supplements at once. Start with one, give it a week or two and if no adverse reaction then add the next one. Again, wait a week or two and if no adverse reaction add the next one. Continue like this. If you do have any adverse reaction then you will know what caused it.
Oh is there? I can’t find it on there
Do you mean your name and NI number? Bottom right hand side of sheets.
Ok thankyou! I shall remove them!
Do you know anywhere I could go to get looked after better? Maybe private places or anything like that?
Do you know anywhere I could go to get looked after better? Maybe private places or anything like that?
No sorry. Private doctors are expensive - consultation fees, blood tests (not all will accept tests that you may do with a private testing company unless done through them which costs a lot more), private prescriptions, cost of private medication, etc. There's no saying that they will be any better than an NHS GP, they're all trained by the NHS originally unless you consult an holistic practioner. If you want recommendations then make a new post on the forum, also you can send for the list of thyroid friendly endos (NHS and private) from ThyroidUK:
email tukadmin@thyroiduk.org
plus they have a list of private GPs and practioners but they are not recommendations. If you would like this list then click on the please contact us link here:
thyroiduk.org/help-and-supp...
Don't forget that there are many experienced hypo patients on the forum who have gone through a very similar journey to you, we all share our experiences so you can gain a lot of information from asking questions here and reading others' posts.
That’s brilliant thankyou sooo much for all the information, honestly I would have just carried on as normal, thinking it was ok to still be tired and stuff.
The reason I ask for that is because I feel I need a full list of what to take and when and how I’m actually getting on as you can tell my doctor doesn’t really talk to me much or seem to be very well educated on thyroid/nutritional health .
The reason I ask for that is because I feel I need a full list of what to take and when and how I’m actually getting on
Generally you will be able to get useful comments from members here, just post with any test results (include reference ranges) and let us know what supplements/dose you are taking. If unsure of how to prepare for tests (timing, leaving off supplements, etc) just ask and someone will respond.
Looking at previous posts
You’re currently taking 100mcg Teva levothyroxine
Request 25mcg dose increase in levothyroxine up to 125mcg daily
You might want to consider trying different brand levothyroxine unless you are lactose intolerant
Teva brand upsets many people
Obviously if you have only ever had Teva difficult to know, unless try, if another brand would suit you better
Most easily available (and often most easily tolerated) are Mercury Pharma or Accord
Mercury Pharma make 25mcg, 50mcg and 100mcg tablets
Accord only make 50mcg and 100mcg tablets
Accord is also boxed as Almus via Boots, and Northstar 50mcg and 100mcg via Lloyds ....but Accord doesn’t make 25mcg tablets
beware 25mcg Northstar is Teva
List of different brands available in U.K.
thyroiduk.org/if-you-are-hy...
Retest thyroid levels again 6-8 weeks after dose increase
GP very poor not to have prescribed vitamin D
But you’re better off taking your own higher dose
GP would only have prescribed 1600iu daily
Retest vitamin D yourself twice year when supplementing
Hi can you explain why I need to increase please? Just so I can explain to my doctor why I am requesting it.
Also how does Teva upset people? In what way? I feel I’ve been ok on it, however I feel anything would have helped the way I first felt because I was so hypothyroid, any levo would have made me feel good.
I’m unsure how to change brands though, so I request it from my pharmacy or do I go to a different pharmacy that has the other brands?
Thankyou for your help! 😊
Suggest you stick with Teva at the moment
As best to only make one change at a time
First step is to get dose increase in levothyroxine and retest in 6-8 weeks
TSH should be under 2 as an absolute maximum when on levothyroxine
gponline.com/endocrinology-...
Replacement therapy with levothyroxine should be initiated in all patients to achieve a TSH level of 0.5-2.0pmol/L.
NHS England Liothyronine guidelines July 2019 clearly state on page 13 that TSH should be between 0.4-1.5 when OPTIMALLY treated with just Levothyroxine
Note that it says test should be in morning BEFORE taking levothyroxine
Also to test vitamin D, folate, B12 and ferritin
sps.nhs.uk/wp-content/uploa...
Graph showing median TSH in healthy population is 1-1.5
web.archive.org/web/2004060...
Aim is to bring a TSH under 2.5
UK guidance suggests aiming for a TSH of 0.5–2.5
As SlowDragon has mentioned regarding Levothyroxine brands. This change in brands alone for me was enough to bring my TSH right down, it obviously was stopping absorption.My surgery no longer prescribes me lactose free brands knowing this.
I also actually got under my right rib pain which disappeared completely when I stopped taking the lactose free brands.
Unknowingly until I came on this forum didn’t know these brands along with their additives could make such a difference, we are all different but it’s definitely something to consider and simple to change.
In a couple of months after settling on new increased dose
If wanting to change brand as trial
You can ask pharmacy for different brand
Perhaps start with Mercury Pharma as has 25mcg, 50mcg and 100mcg tablets available
Once you find out which brand suits you best you can request GP specify on all future prescriptions
gov.uk/drug-safety-update/l...If a patient reports persistent symptoms when switching between different levothyroxine tablet formulations, consider consistently prescribing a specific product known to be well tolerated by the patient. If symptoms or poor control of thyroid function persist (despite adhering to a specific product), consider prescribing levothyroxine in an oral solution formulation.
Many patients do NOT get on well with Teva brand of Levothyroxine.
Teva contains mannitol as a filler, which seems to be possible cause of problems. Teva is the only brand that makes 75mcg tablet. So if avoiding Teva for 75mcg dose ask for 25mcg to add to 50mcg or just extra 50mcg tablets to cut in half
But for some people (usually if lactose intolerant, Teva is by far the best option)
Teva, or Aristo (100mcg only) are the only lactose free tablets
Most easily available (and often most easily tolerated) are Mercury Pharma or Accord
Mercury Pharma make 25mcg, 50mcg and 100mcg tablets
Accord only make 50mcg and 100mcg tablets
Accord is also boxed as Almus via Boots, and Northstar 50mcg and 100mcg via Lloyds ....but Accord doesn’t make 25mcg tablets
beware 25mcg Northstar is Teva
List of different brands available in U.K.
thyroiduk.org/if-you-are-hy...
Posts that mention Teva
healthunlocked.com/search/p...
Teva poll
Just a comment about your above range creatinine this is an area I’m interested in.I too have this, slightly lower than yours at present but has been in 109 but all the same it’s above range.
I’m sure there’s a thyroid link with this unless there’s something else your GP is suggesting.
Just point out I was asked to make sure I’m hydrated prior to my blood test 24hrs before and cut back on my protein at least day before, apparently this can raise it… however mine has never fell enough to be in range but has made a slight difference.
I’ve had a kidney/bladder scan and my urine tested and all fine all other tests are good.
This anomaly bugs me and I’m down as having stage 2 odd times 3a kidney disease and it’s purely as far as I can see is based on my creatinine results.
I had creatinine tested prior to being hypothyroid and was well in range.
I’m asthmatic and had these blood tests done annually a decade before I was hypothyroid and all was ok.
I’m now trying to link this with my muscular problems and hypothyroid myopathy.
I’m interested to know if you get any musculoskeletal problems?
I can see your TSH is high and when my TSH is higher my creatinine goes up.
Anyone else reading this if they could pass on any literature regarding this connection I’d appreciate it.
Apologies for jumping in on your post it was just as your results resonated with mine.