Subglottic Stenosis in Adults Treatment & Management
18 April 2017
Problem
Partial or complete narrowing of the subglottic area may be congenital or acquired. The problem is rare and challenging, affecting soft tissue and cartilage support.
Iatrogenic injuries cause most of the problems seen. Often, subglottic stenosis has an insidious onset, and early manifestations are usually mistaken for other disorders (eg, asthma, bronchitis).
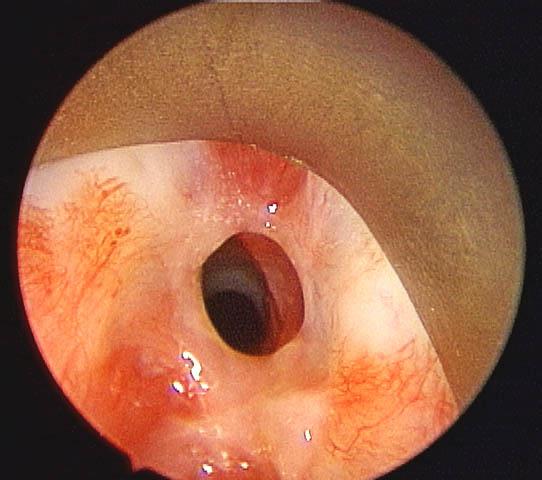
An image depicting subglottic stenosis can be seen below.
Preoperative view of subglottic stenosis via an endoscopic approach.
Etiology
Congenital
Stenosis is said to be congenital in the absence of a history of intubation or other acquired causes. Congenital laryngeal webs account for approximately 5% of congenital anomalies of the larynx, with 75% occurring at the glottic level and the rest occurring at the subglottic or supraglottic level. Most severe cases are diagnosed in childhood.
Acquired
Trauma is the most common cause of stenosis in both children and adults. Approximately 90% of all cases of acquired chronic subglottic stenosis in children and adults result from endotracheal intubation. The reported rate of stenosis following intubation ranges from 0.9-8.3%.
Intubation causes injury at the level of the glottis due to pressure between the arytenoid cartilages. Intubation causes injury in the subglottis due to the complete cartilaginous ring or can cause injury distally in the trachea. Pressure and/or motion of the tube against the cartilage framework may cause ischemia and necrosis.
Duration of intubation is the most important factor in the development of stenosis. Severe injury has been reported after 17 hours, but it may occur much sooner. A 7-10 day period of ICU intubation is acceptable, but the risk of laryngotracheal injury increases drastically after that.
Size of the tube is also important. Tubes should be no larger than 7-8 mm in internal diameter for adult males. Tubes should be no larger than 6-7 mm in internal diameter for adult females. The size of the endotracheal tube needed correlates best with the patient's height.
Stenosis could also be secondary to foreign body, infection, inflammation, or chemical irritation. Respiratory epithelium is susceptible to injury. Initial edema, vascular congestion, and acute inflammation can progress to ulceration and local infection with growth of granulation tissue. Finally, fibroblast proliferation, scar formation, and contracture can occur and result in stenosis.
Systemic factors may increase the risk of injury and include the following:
• Gastric acid reflux*****
• Chronic illness
• Immunocompromised patient
• Anemia
• Neutropenia
• Toxicity
• Poor perfusion
• Radiation therapy
Other causes include the following:
• External trauma, penetrating and blunt
• Tracheotomy, especially a high tracheotomy or cricothyroidotomy
• Percutaneous tracheotomy (This has an emerging role as a cause.)
• Chondroradionecrosis after radiation therapy; may occur up to 20 years later
• Chronic infection
Chronic inflammatory diseases include the following:
• Wegener granulomatosis
• Sarcoidosis
• Relapsing polychondritis
• Chronic inflammation secondary to gastroesophageal reflux and other conditions
• Neoplasm
A study by Gnagi et al found that time to diagnosis differed significantly between patients with acquired subglottic stenosis and those with idiopathic subglottic and tracheal stenosis. While 32% of the acquired stenosis patients were diagnosed within 3 months of symptom onset, just 2% of the other group were diagnosed within this time. The study involved a total of 160 patients.
Pathophysiology
Congenital stenosis has two main types, membranous and cartilaginous.
In membranous stenosis, fibrous soft tissue thickening is caused by increased connective tissue or hyperplastic dilated mucus glands with absence of inflammation. Membranous stenosis is usually circumferential and may extend upward to include the true vocal folds.
In cartilaginous stenosis, a thickening or deformity of the cricoid cartilage most commonly occurs, causing a shelflike plate of cartilage and leaving a small posterior opening. Cartilaginous stenosis is less common than membranous stenosis.
Acquired subglottic stenosis is secondary to localized trauma to subglottic structures. Usually, injury is caused by endotracheal intubation or high tracheostomy tube placement. If irritation persists, the original edema and inflammation progress to ulceration and granulation tissue formation. This may or may not involve chondritis with destruction of the underlying cricoid cartilage and loss of framework support.
When the source of irritation is removed, healing occurs with fibroblast proliferation, scar formation, and contracture, leading to stenosis or complete occlusion of the airway.
Presentation
Adults with mild congenital stenosis are usually asymptomatic, and they are diagnosed after a difficult intubation or while undergoing endoscopy for other reasons.
Patients with acquired stenosis are diagnosed from a few days to 10 years or more following initial injury. The majority of cases are diagnosed within a year. Symptoms include the following:
• Dyspnea (may be on exertion or with rest, depending on severity of stenosis)
• Stridor
• Hoarseness
• Brassy cough
• Recurrent pneumonitis
• Cyanosis
Many patients would have been diagnosed with asthma and recurrent bronchitis prior to discovery of stenosis. A high index of suspicion is warranted with the onset of respiratory symptoms following intubation, regardless of the duration of intubation.
Indications
Indications for treatment are to improve compromised airways and progress toward decannulation. Speedy intervention prior to cartilage damage or scar contracture is preferred when the diagnosis is made early.
Relevant Anatomy
The subglottic area is circumferentially bound by the cricoid cartilage, which is part of the larynx. The adult trachea is 10-13 cm long and 17-24 mm in diameter and extends from the inferior border of the cricoid cartilage to the carinal spur.
The first tracheal cartilage is partly inset in the lower border of the cricoid and, on occasion, may be fused with it. All of the tracheal rings are incomplete posteriorly.
Primarily, arterial supply to the larynx comes from branches of the superior and inferior thyroid arteries. The superior thyroid artery sends a superior laryngeal branch through the thyrohyoid membrane. The inferior thyroid artery sends an inferior laryngeal branch with the recurrent laryngeal nerve to enter the larynx near the cricothyroid joint.
The tracheal blood supply is segmental. Branches of the inferior thyroid artery supply the upper trachea. Branches of the bronchial arteries, with contributions from subclavian, supreme intercostal, internal thoracic, and innominate arteries, supply the lower trachea. The branches arrive to the trachea via lateral pedicles.
Sensory innervation to the subglottic mucosa is by the recurrent laryngeal nerve. The thyroid gland is adherent to the trachea at the second and third tracheal rings, but the lateral lobes overlie the cricoid cartilage and can approximate the lower lateral thyroid laminae.
Contraindications
Most contraindications are relative and include the following:
• General medical state of the patient precluding general anesthesia
• Factors affecting wound healing (eg, diabetes mellitus)
• Active inflammatory state (eg, Wegener granulomatosis); relative contraindication to surgical intervention and warrants medical treatment
• Any active infection at the site; should be medically managed
Contraindications specific to long-term tracheostomy are debatable and include the following:
• Circumferential scarring with cicatricial contracture
• A scar greater than 1 cm in vertical height
• Loss of cartilage
• History of severe bacterial infection associated with tracheostomy
• Posterior glottic stenosis with arytenoid fixation
• Prior radiotherapy (relative contraindication)
Contraindications reported for open repair include the following:
• Contraindication to general anesthesia
• Need for tracheotomy
• Significant gastroesophageal reflux
Laboratory Studies
See the list below:
• In the absence of a history of prior trauma or when suggested by other findings, evaluate for inflammatory or infectious causes, including the following:
○ Wegener granulomatosis
○ Relapsing polychondritis
○ Syphilis
○ Tuberculosis
○ Sarcoidosis
○ Leprosy
○ Diphtheria
○ Scleroma
Imaging Studies
See the list below:
• Radiography
○ Standard chest radiographs can often provide a great deal of information regarding the tracheal air column.
○ Anteroposterior filtered tracheal views and lateral soft tissue views of the neck provide specific information regarding the glottic/subglottic air column.
• MRI is useful in evaluating length and width of the stenotic region by means of coronal and sagittal views.
• CT scan
○ CT scanning is not as helpful as MRI because its views are generally only in the axial plane.
○ Thin cuts (1 mm) with sagittal and/or coronal reconstructions may be helpful, however. This is the preferred initial imaging study of the author.
○ New software allows virtual bronchoscopy, which may be helpful in assessing the airway and surgical planning prior to actually performing a procedure.
Other Tests
See the list below:
• Flow-volume loops do not offer more specific information regarding stenosis than what is gained from imaging. However, flow-volume loops may be helpful in monitoring for restenosis after intervention.
Diagnostic Procedures
See the list below:
• Videostrobolaryngoscopy is extremely helpful in evaluating the glottic and supraglottic larynx for possible concomitant injury.
• Visualization of the larynx by flexible fiberoptic or rigid telescopic (90- or 70-degree scopes) in the clinic is crucial to the evaluation of airway lesions.
Medical Therapy
See the list below:
• Any underlying medical cause must be addressed (eg, control of infectious etiology, inflammatory causes such as Wegener granulomatosis).
• Antireflux management *****
○ Proton pump inhibitor (eg, omeprazole, 20 mg PO bid or equivalent)
○ Ranitidine, 300 mg PO bid-qid, if proton pump inhibitor is not an option
○ Dietary and lifestyle modification; crucial but often overlooked in antireflux management
○ Use of systemic steroids in early stenosis is an option but has not been thoroughly investigated.
○ In active inflammatory states of the subglottis, such as granulation tissue, inhaled steroids are of potential benefit (eg, Flovent 220, 2 puffs twice a day for 2 weeks; this is an off-label use based on the author's own experience).
Surgical Therapy
See the list below:
• Long-term tracheostomy
• Long-term intraluminal stent
• Endoscopic repair
○ Not indicated following blunt or penetrating neck trauma
○ Advocated as a preferred initial approach in chronic subglottic stenosis
○ May require several procedures to obtain desired result
○ Carbon dioxide laser is very useful in this setting, or neodymium: yttrium-aluminum-garnet (Nd:YAG) laser can be used.
○ Airway management may be via supraglottic jet ventilation, intermittent apneic technique, spontaneous ventilation, or a laser safe tube through an already established tracheotomy tract.
○ Triamcinolone injected into the stenotic wound or a topical aziridine compound such as mitomycin C has the potential to reduce fibrosis and can be used in the operative setting.
○ Growing evidence shows efficacy of dilation of the stenotic area as being very helpful.
§ Traditional rigid dilators ("Olive" or Jackson tracheal dilators) are effective in dilation, but they often shear the mucosa, creating a potential for cicatricial contraction.
§ Newer balloon dilators may offer an advantage of dilation without shear.
• Open Repair
○ Open repair is indicated following failure of the endoscopic approach when extent of stenosis is severe or factors are unfavorable for this approach.
○ Choose the specific technique based on length of resection, need for cartilage, and need for mucosal coverage.
○ Stent placement is required in some procedures.
Other procedures
These include the following:
• Anterior cricoid division with interposition graft (eg, hyoid-sternohyoid muscle, split clavicle muscle, rib)
• Anterior and/or posterior cricoid split with stenting
• Anterior laryngofissure with anterior lumen augmentation
• Trachelopexy with muscle-fascia repair
• Resection of stenotic segment with end-to-end repair
• Staged free-graft repair
A study by Deckard et al indicated that, as in pediatric patients, two-stage laryngotracheal reconstruction (LTR) can be successfully used to treat subglottic stenosis in adults, offering a means to avoid the complications of cricotracheal resection. In the study, 14 adult patients, most of whom had high-grade (grade III or IV) stenosis, underwent LTR, with 12 of them achieving decannulation. One of these patients, however, subsequently required salvage surgery and was decannulated again only after cricotracheal resection. Thus, 11 patients (79%) achieved decannulation with LTR alone. [3]
Preoperative Details
See the list below:
• The length of stenosis, its severity, involvement of cartilage, and degree of scar maturity must be known prior to any attempts at repair. The endoscopic approach has a high failure rate if the stenosis is longer than 1.0-1.4 cm.
• Detect any proximal or distal injuries (eg, supraglottic stenosis, posterior glottic scar, arytenoid fixation, distal tracheal stenosis).
• Use imaging and endoscopic investigation.
• Begin antireflux management approximately 1 month prior to repair.*****
Intraoperative Details
In the endoscopic management of the stenosis, mitomycin-C has become routinely used. The concentration is usually 0.4mg/ml and is applied topically on a cottonoid pledget. The length of application varies from 2-3 repeat applications of 2 minutes each to a single application of 5 minutes.
The handling and disposal of the mitomycin-C should be per the hospital protocol for chemotherapeutic agents. Care should be taken to avoid contact with unprotected skin.
Postoperative Details
See the list below:
• Endoscopic Approach
○ Antibiotics for 1-3 weeks, depending on wound extent and general health of the laryngotracheal mucosa
○ Intensive antireflux management *****
○ Wound reassessment in 6 weeks to determine state of healing and need for further procedures
Postoperative view of subglottic stenosis after 4-quadrant carbon dioxide laser division and endoscopic balloon dilation. Note the excellent view of distal airway.
View Media Gallery
○ Tracheostomy care if applicable
○ Inhaled steroid sprays (not nasal sprays) are sometimes useful to reduce granulation tissue at the surgical wound.
• Open Approach
○ Admit patient into an ICU setting.
○ Administer antibiotics appropriate to the surgical repair and wound bed.
○ Some authorities advocate suppression antibiotics when a stent is used.
○ Initiate antireflux management. *****
○ The role of postoperative intubation still is controversial.
○ Some authorities desire immediate extubation postrepair; some support 1-2 days of postoperative intubation in the ICU; and some require extubation in the operating room rather than in the ICU.
○ Some recommend prolonged postoperative neck flexion by splint or chin-to-chest suture in an end-to-end anastomosis.
Follow-up
See the list below:
• At least 1-2 years of postrepair evaluation as the scar continues to remodel and mature
• Symptomatic and/or flow-volume loop evaluations
• Imaging in questionable cases
• Capping trials and endoscopy prior to decannulation if tracheostomy is present
Complications
See the list below:
• Mucus plug occlusion
• Wound infection or abscess formation
• Granulation tissue formation
• Bleeding/hematoma
• Subcutaneous emphysema
• Pneumothorax and/or pneumomediastinum
• Stent problems (eg, migration, breakage)
• Reformation of stenosis
• Injury to recurrent or superior laryngeal nerves
• Airway obstruction
• Death
Outcome and Prognosis
Overall goals are improvement of airway function and preservation of laryngeal function. The endoscopic approach was found to be successful in 57-90% of cases. Intraluminal stents were found to be successful in 80% of cases.
In a study of 109 patients with subglottic stenosis, D’Andrilli et al reported that the long-term results of laryngotracheal resection demonstrate it to be the definitive curative treatment for the condition, with 94.5% of the patients having good to excellent outcomes from the surgery. [4]
Open Approach
End-to-end anastomosis was found to be successful in 80-90% of cases. Mortality was reported at 10-20%; it has decreased with experience. Morbidity is 20-50%, secondary to the effect on laryngeal function and swallowing.
Augmentation Techniques
Successful case rates of 60-96% have been reported. Grafts are susceptible to infection, resorption, displacement, and extrusion.
Author: James D Garnett, MD; Chief Editor: Arlen D Meyers, MD, MBA
© All Rights Reserved
Note: In addition to the G Reflux connection there is another potential association via the recurrent laryngeal (left) nerve which can be impacted in an Ivor Lewis procedure entailing a cervical anastomosis. [GW 18/4/207] *****