Hi every body. I am 38 yrs old female .This was my mri spine lumbar report. I am in lower back pain . When move or climb stairs or even sit down or stand up I feel like my back is broken and thunder like pain . I am at the 3rd floor and I am not being able to go any where to avoid stairs since weeks . I keep complaining the pain 😪 the GP referred me to physiotherapy regarding to my MRI but they said my MRI does not show any reason for this pain . 😔 and I have urine incontinence as well. Would any one please read my MRI report .. thanks a lot 🙏
MRI spine lumbar: Hi every body. I am... - Fibromyalgia Acti...
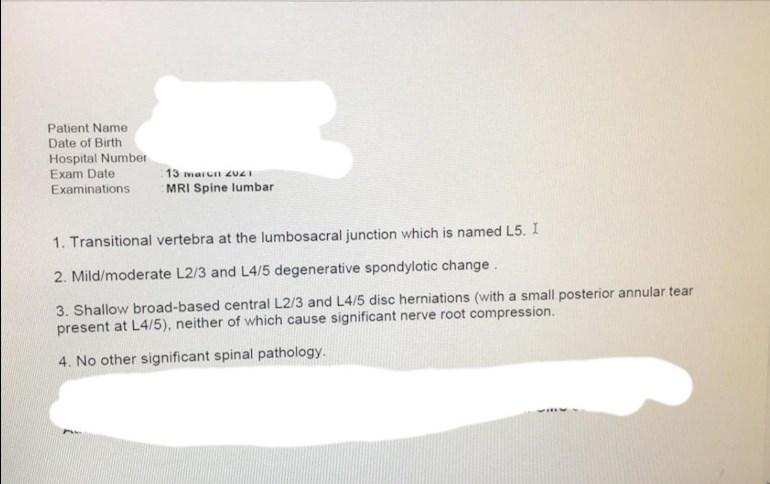
MRI spine lumbar
Hi, we are not medically qualified to read your mri report. You would be best speaking to the doctor who requested it for an explanation
Questions to ask gp and anyone else’s ear you can grab. I’ve had similar results and the incontinence as well. Depending on the notes that were in the requested mri of what to look for could be a reason to ask more questions. Some gps write to look in as pacific area, not to use the opportunity to delve into other regions. The incontinence could be attributed to a injury or issue on an area out of the mri view. Asking your gp if you need to see someone (gyno and a physio) that deals with pelvic and incontinence is good. Inflammation in the area or weak muscles from overcompensating others do to the pain you have you could be aggravating it more. Physio helped me get back into shape and are addressing the deeper issues finally. They even helped with occupational therapy to show me how to move and sit when I’m having a flare to not aggravate it. Follow up with the gp or an orthopedic to get answers and information on what your results mean. I’m in the US so I’m not sure what doc specialists you have available for it. When you do start physio, ask questions, if one move is easy, but another is painful ask why. The more you know about your body the better you can ask your gp or whomever else about it as well.
What it’s basically saying is … your Lower 3 discs have degenerative disease, simply put there getting older quicker than you. One disc has a rupture and another slightly out of place, slipped disc. BUT In his opinion it’s not causing you pain. I’d question that ? As if it’s out of place it swells then goes back down so your MRI might only be showing it in a non swelled state. Also one is ruptured how can they tell the pain is not coming from there ? As your GP. I started out a bit like that and kept working through the pain with pain killers. I wish I hadn’t. But this isn’t about me.
Id speak with your GP and ask for some pain relief for your pain and ask about your other problems too. It’s going to be trial and error for a while but bear with your GP while he/she tries to find a relief that works best for you.
It’s going to be harder now because of them not prescribing pain killers like they used to. I’m sort of last hope now on Morphine but it’s been working great. So stick in. It’s a bit of a long haul but I’m sure you’ll get there. In the end.
Hi u know how your body, sound like your not happy with your gp so request to see a specialist to put your mind at rest phiso will be good , I know its bad and u r young this is what I do it might help keep moving treat your self to a soft cocix / pressure cushion that will help with pressure when sitting use cold gels and heat pads its won't fix the problem just to Diss stract for a short time all the best Angela
Apparently many people who aren't in any pain would get similar results in an MRI. They for years mixed up correlation with causation, it's only when they gave MRI's to people who weren't in pain they started to find similar test results and realized they needed a rethink. This is in part why NICE have instructed doctors to not prescribe opioids for back pain and fibromyalgia.
Well you say that but my GP and my daughter’s doctor have both prescribed morphine and patches for the pain.So, I am unsure why some do and some don’t. My back is also very bad, some days it feels like it’s actually broken in 2.
I've been prescribed morphine even though they know it doesn't work on fibromyalgia so I wouldn't put much store in that. I know people can have bulging discs and not feel any pain and they don't understand why some people do and why some don't. Its the same for people with weak core strength, it's often attributed to back pain but there are plenty of people with no core strength that don't suffer back pain.
Well it most certainly does work on my pains and for my daughter.A good friend suffers too and has admitted without his morphine he wouldn’t be able to get up in the morning
The trouble with morphine is it will relieve your bodies need for more morphine so there is always a cycle of pain and relief with morphine which makes it hard to distinguish between that and the original pain. It can confuse the picture and when you are desperate for pain relief, which obviously most of us are, you don't always care about why and how it comes just that it comes in some way. For sure it can alleviate short term pain but learn term it's not so effective, withdrawal is always painful.
I’m sorry but I disagree with what you’ve wrote 100%.
It’s been over 30 years since my accident at work when the scaffold collapsed with me on it and I relive every moment when I’ve not got pain relief.
For the past eight years I’ve been on morphine gradually working up to that strength of pain relief. I was told at the time it will only ever get worse. Sure they have tried everything but nothing has lasted longer than a few weeks of relief. I’ve also worked throughout that has in fact made things worse quicker.
I’ve gotten on a dose that works for me and gives me my life back. I’ve never had this, feeling of getting high where your meant to float and your head spins. To me that’s a myth. All I feel is the pain gradually going away. I’ve been on the same dose now for years now so the other part of the theory where you crave more doesn’t work on me either although saying that there is a 2 to 2 1/2 hour period every morning and every night that I’m in pain since it was reduced a few years ago. I would have liked that one pill back but they say it just takes you over that Oxford papers limit. Which I find ridiculous that it should be such a hard and fast rule. Everyone is different where medication is concerned.
Yes I'm sure there will be many that disagree with me 100%. My opinions on this are not for a 100% of people anyway, as you say we are all different. If you have PTSD from your accident there is another layer of complexity. I think the reason morphine is not supposed to be good for fibromyalgia patients is that we have few opioid receptors therefore it doesn't work very well on us but obviously the logic would be that some people have plenty of opioid receptors and so they will have a much better response. Also when I am thinking of "long term" use I'm talking 30 years plus. From an anecdotal point of view I know a few people you have been on it this long. They say it has no positive effect on their pain anymore but they keep taking because they can't cope their condition and the withdrawal. And I also have two close friends who have been told that morphine has damaged their hearts which they are angry about because they weren't warned abut the negative side effects. One of them is in stage 4 heart failure and they are still giving her morphine and she is only 32, but when her pain levels get too high her heart starts to malfunction more so she's in a catch 22 situation.
Hi, sorry your in so much pain, I have the same degenerative back problems and osteo arthritis in my back and because of this it often becomes inflamed and swells which then can put pressure on the nerves surrounding the damaged area and that causes pain, you could try either a lidocaine patch or ask your dr if he would prescribe for you morphine patches, obviously this won’t fix your problem but may help with pain.
I had an MRI on cervical & thoracic spine 7 months ago due to agonising pain. Similar outcome to you: old age not the cause of the issues. Over the last 7 months it has become clear that it is movement that triggers the debilitating changes so I have saved up & am paying for a private MRI next week BUT the difference is this is an upright MRI that has what is called varipose. This means that they put you into different positions so that they can see what happens when you move. I wrote to them about having this & they did ask why I wanted a further MRI if I had had one. Once I explained they were happy to proceed. You don't need a GP to refer but you do need to give a GP name as they will send the report to the GP as well as you as it needs to be attached to your medical records. Now I'm not saying that this is what you should do (everyone's case is different) but what I would suggest is that you discuss with your physio whether such a test could help in treatment/diagnosis (they may say they think it will make no difference whatsoever)? These are the people I am using (2 centres Manchester and London) but I'm sure there are others out there though I simply don't have the energy or resilience to go looking. medserena.co.uk/mri-scans It is incredibly difficult when a test comes back to tell you that the pain you are in is not caused by what they have tested for yet your symptoms are life changing. This tells me that they're missing something but unfortunately with the NHS as it is in the UK it means that they stop looking for the cause and try to minimise the symptoms. I'm not yet willing to accept that but of course when I can no longer save for tests, I will just have to.
This is awesome! I’m in more pain standing and sitting than laying down. Just left a message with my gp to see if I can get one done! I’ve always tried to position to have a pain when getting scanned so they can see it on the film but alas, not enough to warrant further tests. Had neck X-ray yesterday and had me tilt head back as far as I could, she was in shock how far I could go, she had me lift a little. I fussed that if there’s a reason I shouldn’t be able to do that you won’t know without it being on film! Oi…
Same for me. In fact I know that two things that trigger a flare up is: typing (because my shoulders drop forward) and asymmetrical overhead work (such as cleaning my dado rail which is why today I am doped up on pain meds due to 15 mins of cleaning yesterday)! I am hoping that the upright MRI will either it will tell me that there is nothing observed which means it is not coming from the spinal region & so I'm off down the musculoskeletal pinching of nerves (likely vagus nerve for me) or they will tell me they've found something. Either way I think it's worth it as I'd really like to be able to be active for more than 15 mins without having to pay for it for the next 10-14 days. The real advantage is not having to go through the GP because unfortunately for me I've found that they're much more willing to give me pill after pill after pill but not to put me in front of someone/do something that may actually give us answers.
Doesn't look a million miles from my scan results which would 'probably require surgery' from a private consultant, then 'need no further action' from the NHS consultant. Irony is, they're both the same guy!
After two years of relentless cage rattling I'm lucky enough to have started losing my toes due to a quirk of peripheral neuropathy. This bumped me up the urgent list and now I'm being ignored directly by the consultant rather than via my GP.
The NHS. A Health system for Namibia to be proud of.
Ranting aside, we are all wired differently. If it's causing you pain it needs treatment irrespective of their dismissal. Read the patients charter and arm yourself with a few quotes. And ring and email everyone daily until they get sick of you. I sat in reception for 3.5 hours just to make a booking once. But they respond to whomever is the largest rectal irritant.
Good luck. Don't suffer in silence.
Hi, I’m new here but had to reply, I was accused of being a serial attender by a guy I saw at hospital who was 6 months off finishing his training to become a dr so I do now think NHS stands for no health system I now won’t go near them
Have you seen a cronic pain specialist ? Thats my next step always have pains so brutal i think i wont make it one more day i had a bunch of mri /xray , yours sounds alot like my results nothing much they can do but physio which can add up quickly , im in canada so things arent as advanced as the UK , but i was told osteoarthritis and spinal scoliosis. As you grow things change my doctor told me ! Always fun ..NOT
Same for me, told me pain clinic was all they could offer but when I looked into the difference btwn a 'lay down' MRI it seemed obvious that something that had peaks and troughs of pain levels would be something that could be affected by posture (I mean that in a movement rather than specifically bad posture way). Unfortunately this means that any lay down MRI wouldn't pick it up but of course as I said in my earlier post, this may not be the case for you & it may be that the laydown MRI should've picked up any issues. I'm always reading these posts to get ideas on what I might want to do next then sit down and reflect on whether their circumstances are similar to mine, consult with my private physio (NHS physio pointless as they've 'bought the farm' telling me 6 sessions of physio & I'm a fail and off to the pain clinic) then make a decision. If nothing else, for me it helps me get to a place where if I need to accept this is as good as it gets I'm not left wondering what if ...
I have got the same problem
Hi, I feel for you. Did the incontinence come on at the same time as the back pain if so you really need to make this clear to your GP and if you can ask to see a consultant asap to rule out a link.
I guess if you have had an MRI you have been waiting with this a longtime?
MRIs in my experience they need to be interpreted by a spinal consultant as well as by the radiographer, similarly X-rays. The consultant will put both together along with his own assessment of your symptoms and medical data. The resolution of current MRI is about a mm so a lot of the fine detail from the nerves that come out from your lumbar spine such as your sciatic nerve is not good enough. You can see compression and disc herniations but as others have said this does not always in translate to cause and effect. I have been told it's the speed of the event and any resultant compression that influence the pain you get. It might be worth while looking at NICE guidance for low back pain and if you can use this to discuss your situation with the medics
My own personal experience has covered 30 years 2 lumbar fusions 20 years apart, MRIs, x-rays bending, weight bearing, lying, consultants good, bad, private, nhs, pain clinics, opiates, other procedures, feeling in pain, feeling fine, a great job and family, travelling the world, etc.
Things to pass on, get the advice of a spinal consultant as soon as things get serious in terms of how the pain is impacting you and your life, use pain meds sparingly but don't feel any guilt in asking for them/help, your pain is your own, be assertive with yourself and others in tackling it, in some cases surgery does work and it's a lot safer now than it was, keep your fitness and especially core strong, use a water bed if you can = good core and warm in winter, physiotherapy used to be good now they don't like to be so hands on so you might need to find one that suits your situation. Things may seem bad at the moment but that can all change very rapidly and unexpectedly with backs to the better.
B