What if our doctors could recommend IgG replacement therapy (IGIV or subcutaneous IgG) before we became seriously ill, preventing that risk to our health, even our life? Or proactively recommend vaccination boosters or prophylactic antibiotics or antivirals? This is what a CLL specific immunome could provide. Currently, outside of medical research establishments, medical science lacks the ready capability to determine our risk of serious illness from all the infectious disease threats we face. Rather than having standard recommendations of COVID-19 boosters every 6 months for the immune compromised, if we've just recovered from COVID-19 and have developed good hybrid immunity, more specific testing could spare us the minor risk from boosters.
Given CLL compromises our immune system in many ways, healthunlocked.com/cllsuppo... this Ground Truths article by Dr Eric Topol, is extremely relevant regarding the current inadequacies of standard blood testing for measuring our risk of infection!
open.substack.com/pub/erict...
It is startling that here we are in 2024, recognizing how critical our immune system is for protecting us against infections and major diseases, such as cancer, and how it tells us about our aging process (immunosenescence), yet we have no informative clinical test to get at it.
The crude way we can assess our immune system is from a complete blood count (CBC) looking at the white blood cell (neutrophil) to lymphocyte ratio (NLR). It is a very rough assessment of the balance between inflammation (neutrophil count) vs immune system (lymphocyte count) and is associated with a poor prognosis for cancer, higher risk of major cardiovascular events, infection, and all-cause mortality. The associations are statistically supported but of little help for interpretation at the individual level. Accordingly, most clinicians don’t even look at it.
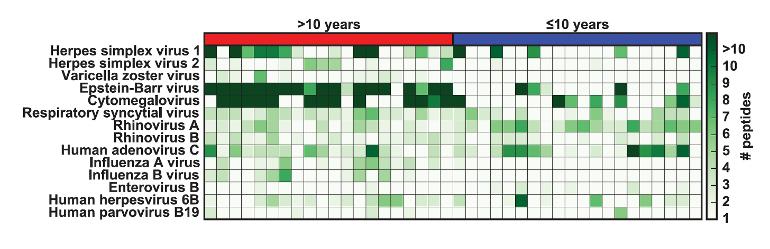
Back in 2015, I was excited about a report in Science on VIrScan. A drop of blood detecting antibodies— to >1,000 virus strains from over 200 species—could tell us about every virus a person has been exposed to and when for as little as $25! A sample of output for 14 virus strains is shown.
:
Throughout the Covid pandemic we’ve seen the importance of T cells—helper CD4+ and cytotoxic CD8+—from research studies, telling us about our immune response to the virus, its many variants, and vaccines. But none of these T cells tests are commercially available. They’re only done in research labs.
:
Immune Health Grade and Immune Resilience
A study that assessed CD4+ and CD8+ cells (immune health grade) and gene expression (transcriptomics) to get at the balance of immunocompetence (IC) and inflammation (IF) for quantifying immune resilience. Think of it as major refinement beyond the neutrophil to lymphocyte ratio.
:
Immune Health Metric (IHM)
Published this month was a study of 228 participants with various genetic immune conditions, along with age and sex-matched healthy controls, with A.I. to derive a score. The immune profiling included complete blood count with B cells, T cells, NK cells, platelets, transcriptomics, proteins, with modules of the RNA and protein data.
Some notes with respect to the above:
1) The white blood cell (neutrophil) to lymphocyte ratio (NLR) doesn't work for us, because our lymphocyte count is typically raised due to our CLL. This is also why checking percentages of white blood cells are so misleading. Because all 5 white blood cell types must add to 100%, when the percentage of lymphocytes increases, the percentage of other white blood cell types must fall, even if they go up a bit less than an increase in the lymphocyte count! See: healthunlocked.com/cllsuppo... This is also why we need to measure our absolute lymphocyte count, not our WBC, to best assess our CLL blood tumour load changes! healthunlocked.com/cllsuppo...
2) The paragraph about T cell testing is extremely relevant to us. Testing for antibodies/immunoglobulins (IgA, IgG, IgM, etc), is very easy, because they are are significant component of our blood plasma protein. Finding T cells with specific T cell receptors for a given virus is far, far harder. Because CLL and CLL treatments inhibit our ability to make immunoglobulins, low immunoglobulin counts (hypogammaglobulinemia) is common with CLL. But because we don't have a VIrScan test available to us (see accompanying graphic), doctors can only use the gross measure of our IgG level, which is not a useful measure of the protection provided to us from illnesses we commonly encounter. That's why being prescribed replacement IgG therapy (IVIG or subcutaneous IgG), requires both a history of a sufficiently low IgG count (the count threshold depends on where you live), as well as some serious, recent infections. It is possible to do blood serum titre tests to check for antibody levels against some infectious diseases, but it's rarely done. The final version of "VIrScan. A drop of blood detecting antibodies— to >1,000 virus strains from over 200 species—could tell us about every virus a person has been exposed to and when for as little as $25", will undoubtedly cost more than $25 as Dr Topol notes in his article. However, it should still be far cheaper than visits to the doctor or a hospital admission, when used to inform appropriate prescription of vaccination updates and prophylactic cover from IgG replacement, antibiotics and antivirals.
We also learned from the COVID pandemic, that immunoglobulin protection from COVID-19 infection is challenging for us to achieve. However, about 80% of us are able to achieve T cell responses to COVID vaccinations/boosters.
3) CLL drives T cells to exhaustion and tends to reverse the CD4:CD8 ratio by driving an increase in CD8 T cell numbers. So measures of Immune Health Grade and Immune Resilience and an Immune Health Metric (IHM) would need to be specific for CLL.
Dr Topol concludes;
Where to Go From Here?
With a large body of knowledge indicating the immune system as a (if not the) major determinant for our health and diseases, we desperately need a means for assessing our immune system. It could predict a person’s response to infections, vulnerability to cancer or its spread, no less cardiovascular and neurodegenerative disease susceptibility. Since our immune system function is quite variable with aging, knowing a person of advanced age is not immunocompetent could lead to ways to augment the immune response. There are diverse means that could be accomplished in the future, such as via the gut microbiome through pre- or probiotics. Or vaccines. Even lifestyle factors such as diet, exercise and sleep are actionable modulators of our immune response.
Perhaps the most striking impact of the immune response relates to treatment for cancer. We have seen notable progress with immune checkpoint inhibitors, but that is often transient, and bolstered with many other strategies to rev up the immune system including CAR T therapy, bispecific T cell engagers (BiTES), cell-drug conjugates, JAK-kinase inhibitors, tumor infiltrating lymphocytes, and neoantigen cancer vaccines. All of these options, and their combinations, are targeting the patient’s immune response to the tumor, but none are directed to the health of their immune system per se. We’re “throwing the book” of immunotherapy treatments and increasing success, but ironically we’re not able to measure the patient’s intrinsic immune system’s status. article is well worth a full read.
As Dr Topol says, "We should accelerate our efforts to get there and build on the promising studies I’ve reviewed."
Meanwhile, appreciating how our immune system works and what we can do to reduce our risk of infection, are very worthwhile endeavours if we want to live out a normal life expectancy with CLL healthunlocked.com/cllsuppo...
Neil
 I've changed the introduction to my post to explain what a CLL based Immunome could offer us. Given infections remain a significant cause of reduced life expectancy with CLL, let's hope that our medical team can soon use something like VIrScan and other tools to proactively reduce our risk from infectious diseases.
I've changed the introduction to my post to explain what a CLL based Immunome could offer us. Given infections remain a significant cause of reduced life expectancy with CLL, let's hope that our medical team can soon use something like VIrScan and other tools to proactively reduce our risk from infectious diseases.