Frightened by falling neutrophils? Worried about being at a greater risk of infection? This is a common and often totally unnecessary fear, simply because standard blood count reports give more emphasis to presenting the percentages* of the different white blood cell types than the absolute counts. They may not even provide absolute count figures. If so, this is the ONLY time you need to look at percentages† , so that you can calculate your absolute counts.
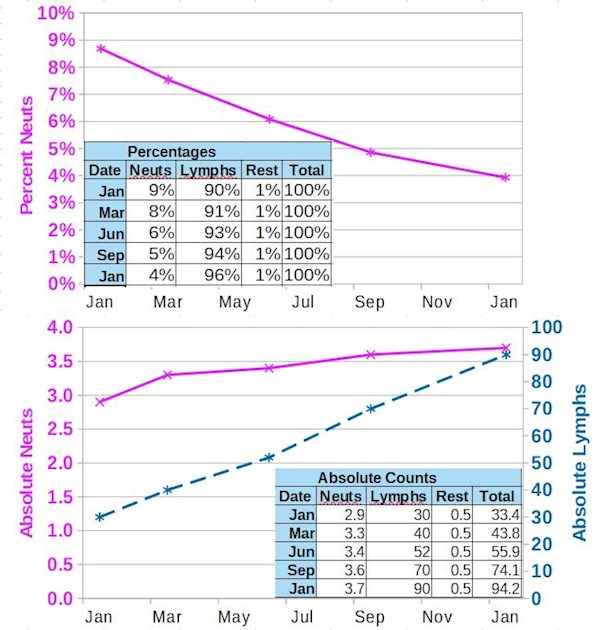
The accompanying image includes two plots from typical results for a CLL patient with a lymphocyte doubling time of about 8 months. The top plot shows neutrophils dropping - or does it? This plot just shows the percentage of neutrophils dropping. If you look at the absolute count plot in the lower plot and in the included table, you'll see that the neutrophil counts are excellent and actually improving! (Purple solid line). That's because with CLL, your lymphocyte count typically rises (dotted blue line) and the total percentages of all the white cell types must add up to 100%. So when your lymphocyte count increases, the percentage of lymphocytes also increases, provided other white cell absolute counts have not changed much. You can't exceed 100% in your total percentage of white cell types, so the other percentages must fall. Neutrophil counts may even increase slightly while their percentage falls, as in this example, where the absolute neutrophil count has risen 28% over the year.
Commonly in blood test reports, the white cell count types are reported in what's termed a blood differential test. This measures the amount of each type of white blood cell (WBC) that you have in your blood sample. There are typically white cell five types listed, here provided in decreasing count order:
- Neutrophils or Segs (normally about 65% of the total) Reference range ~2 to 8
- Lymphocytes (which include CLL cells plus healthy B and T cells and normally about 30% of the total. This is why it is important to monitor your lymphocyte count, not your WBC with CLL: healthunlocked.com/cllsuppo...
- Monocytes
- Eosinophils
- Basophils
(I've lumped these last three types into 'Rest' in the plots above)
I seem to be spending more time lately, reassuring members that they probably do not have a problem with falling neutrophil counts (i.e. at risk of developing neutropenia). Hence this post. It's extremely important to be aware of your neutrophil count, because our neutrophils are so important in keeping us free from dangerous bacterial and fungal infections. During watch and wait, they can fall as our bone marrow becomes more infiltrated with CLL and all CLL treatment drugs carry with them the risk of neutropenia.
Neutrophils quickly respond to infections. They cause a wound to become red and swollen as the neutrophils move out of the blood into the tissue around the wound, where they engulf bacteria and fungi along with dying body cells. When they have done all they can to protect you from infection, they die, forming pus. This post covers neutropenia precautions: healthunlocked.com/cllsuppo...
This video by Dr. Erel Joffee, lymphoma specialist with Memorial Sloan Kettering Cancer Center, recorded for the USA's Leukemia and Lymphoma Society, covers both neutropenic fevers and how to interpret blood counts. Note his words from the 6:38 mark, especially from the 6:50 mark, "You should only look on the absolute numbers. You should look if the absolute numbers are within the reference, not the total number and definitely should not look at the percentages... The percentage of the neutrophils, lymphocytes, monocytes and so forth are completely irrelevant and please do not look at them."
Also note his remark at the 9:21 mark, with respect to absolute lymphocyte counts. "If the patient is asymptomatic, absolute number, we don't care."
A useful analogy for why absolute counts, not percentages are so important is to think of two belligerent countries. If we consider neutrophils as aircraft (air supremacy being so important in warfare), the country with a greater percentage of aircraft in its defence forces would not go to war against its foe if that foe had absolute supremacy in aircraft numbers.
* White cell differential percentages are great for your GP/PCP for 99.99% of their patients. CLL is a rare cancer, so most doctors would only see a few cases in their entire career. The percentage differential provides a quick, at a glance indication of any imbalance in white cells, typically indicating an infection or allergy. However, when you have CLL, percentages do far more to confuse than to help. Ignore percentages and concentrate on absolutes. Please!
† If absolute counts are not provided on your blood test report, you can easily work them out by multiplying the WBC count by the percentage of the white cell you want to know. For example, in the image above, the total WBC in January is 33.4. The percentage of neutrophils in January is 8.7% (rounded to 9% in the table). 33.4 x 8.7% = 2.9, which is the absolute neutrophil count for January.
Blood count tracking spreadsheet templates are available per this post: healthunlocked.com/cllsuppo...
Neil
This post is unlocked/open for discovery on the Internet, it's so important.
healthunlocked.com/cllsuppo...
Last updated 20th November 2021