This is slightly complex but good overview of the acquired resistance mechanisms to novel agents.
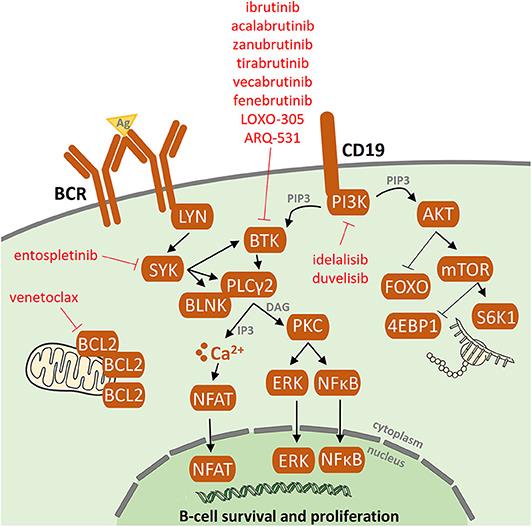
In 80% of patients with ibrutinib failure, acquired mutations in BTK and PLCG2 genes were detected. No common resistance-associated mutations or deregulated signaling pathways have been reported in idelalisib failure. Acquired mutations in the BCL2 gene were detected in patients who had failed on venetoclax.
For 20% of patients, the ibrutinib resistance-associated mutations remain unknown. This data further supports the presence of alternative mechanisms of drug resistance other than BTK/PLCG2 mutations. To date, several candidate loci/mutations that may contribute to resistance have been described. These include del(8p) and SF3B1, PCLO, EP300, MLL2, and EIF2A mutations but these are only generally tested for in a research setting.
Resistance-associated mutations tend to occur between the second and fourth years of treatment and may be detected several months before clinical relapse.
They also discuss the development of next-generation agents for CLL patients who have acquired resistant mutations to current inhibitors.
Much more here if you're interested: frontiersin.org/articles/10...
Jackie