Some excerpts from a podcast covering many aspects of active surveillance, both post radical prostatectomy (RP) and adjuvant/ early salvage radiation (aRT / eSRT). There is an interesting breakdown of usPSA (ultra sensitive PSA) with predictive values for BCR. Last, it appears that the metric of ‘cure’ measured at 5 years for men with RP surgical classification of T3 does not apply, with the chances of BCR never dropping below 30% even 10 years out…
Important, take a look at minute, 10:55…you wouldn’t take your car to a mechanic without experience, so it’s not surprising that it matters who does your surgery. Take a look at the difference in outcomes for surgeons as they gain experience. This is an important point that has to be stressed to any of our brothers coming along. You have to go to a center of excellence and choose a surgeon with more than 1000 surgeries. That sounds like a lot but it’s not. You certainly don’t want to be one of the first ones that is operated on, at least not without a big discount (it’s a joke).
This podcast has a lot of information; review and determine what fits your particular condition. I know these are numbers, but they are based on studies and statistically represent projections of how this disease can progress. Each of us is unique and may not fit the pattern, but what else do we have to help us 1) consider what treatment should follow and 2) determine where we are in the fight against this most unwanted, unwelcomed and detestable guest…Rick
PS this podcast precedes PSMA PET so this diagnostic is not mentioned but looms large in determining what treatment options should be considered...I start my post RP, eSRT, 21 months of ADT 'surveillance,' and my usPSA is holding at 0.006 ng/dl so here we go...
1. 20 to 30% will develop recurrent disease
2. BCR of two types; persistent and recurring. Persistence is when it never goes away. Recurring is what it is initially zero and comes back.
3. Does rising PSA mean cancer; no. Benign glands are commonly seen at margins. Distribution at Apex only or Apex and other is 40% and 73% of the study. Bladder neck base and other was 51% of the study. This is because the prostate shell is deficient or thinnest at the bladder neck and the Apex. It’s the worst place you can get a tumor.
4. Biochemical recurrence in this article is anything over 0.1 ng/mL
5. German study 2004. 74% of men had residual benign glands distal to or on the opposite side of where positive margins were noted. Nerve sparing operations tend to leave behind residual benign glands more than traditional surgery.
6. DAmico Risk classification. Clinical stage high risk is a T3 classification. 50% survival from bio chemical recurrence (BCR) at three years. 30% survival maximum at seven years. It does not get less than 30% even after 10 years.
7. Boorjian Eur Urol 2011; 2424 patients. T3B was 14.5%, Gleason score 7 was 40%, PSM positive surgical margins was 39%. Out of this group 11.7% progressed in the disease 22.9% died but only 5.8% passed away from PCa prostate cancer. Median follow up time was 6.6 years. 15 year PFS progression free survival was 75.8% and CSS cancer survival was 83.6%.
8. Simmons Eur Urol 2007; 13 to 36% of patients with BCR demonstrate clinical progression and only 1.1 to 14% die of the disease with prolong follow up. The follow up is 10 years to 15 years.
9. Summary stats; 2-6 of 100 pst will die of their PCa.
10. Median time between biochemical recurrence BCR and development of metastatic disease METS is eight years. That is with a BCR PSA greater than 0.2 ng/mL.
11. Factors that predict metastasis free survival; Gleason score, time to BCR and PSADT doubling time. Gleason score is a 5 to 7, PSA recurrence after two years and doubling times more than 10 months after recurrence are the best predictor’s for metastasis free survival.
12. Definition of biochemical recurrence. A PSA of greater than or equal to 0.4 and rising with an R2 of 0.21.
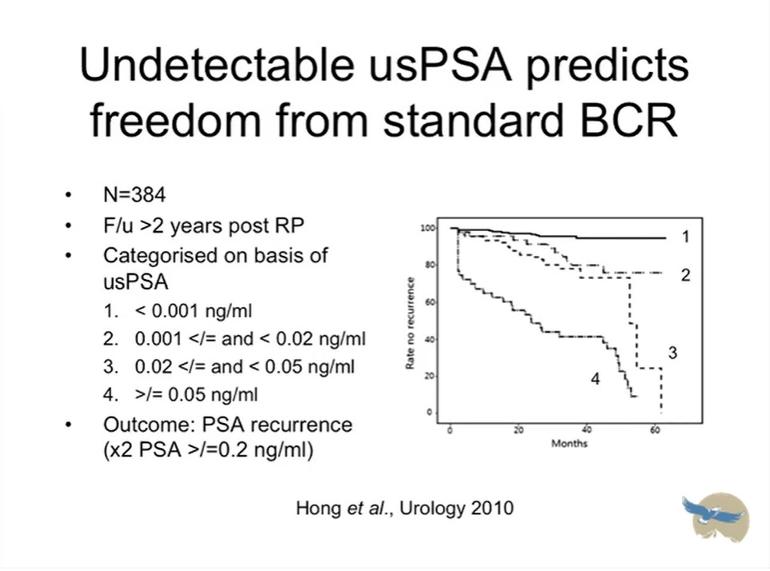
13. usPSA Predictive tool; if your PSA is undetectable at the ultra sensitive level it is a good predictor that you will not have recurrence. Break of usPSA is given; 80% of patients had no BCR after 60 months at levels below 0.02 ng/dl. Once usPSA goes above 0.05 that drops to less than 10% BCR free.
14. Radiotherapy prognostic factors; BCR more likely if you have…
• Gleason score of seven or more
• SVI Seminal Vessel Invasion
• Short PSA doubling time <3Mo
• Negative pathological margins
• PSA persistence versus recurrence
• Palpable prosthetic mass
• Radio therapy RT dose less than 65GY (Grey)
15. Adjuvant RT; Bolla Lancet, 2005. Survival rates are more than 20% better for adjutant radiation therapy then wait and see.
16. Arguments in favor of adjuvant radiation therapy aRT. Most occurrences happen in the prostate bed (called clone cells) and if you don’t treat the cells differentiate and spread. So the best place to start the treatment is with adjuvant therapy in the prostate fossa.
17. Data comparing aRT versus early salvage radiation therapy. There is no difference in the long run. But the Nomogram assumption that the early salvage failures will respond 50/50 to salvage radiation. Without this assumption aRT still appears superior.