Hello, I have posted before regarding my daughter who is 10yo but we have just had some very unusual and worrying results which may explain her health issues. She has a long term history of low platelets and I’ve been trying to solve this for her as it has been unexplained. We have strong family history of thyroid disease (she also has DIO1 single/DIO2 double defects) plus a few family members on B12 injections (none have had pernicious anaemia or issues with intrinsic factor discovered though. I am currently going through the motions for B12 investigations as my active B12 is at the bottom of the range).
My daughter has had her low platelets diagnosis since 2016 when she was about 3/4 yo but it could have been from earlier in life. During birth which was very traumatic for her, I had probably been on gas and air (which depletes B12 stores) for near enough 24 hours. During her first year of life she was put on omeprazole (a strong dose) because she could never settle (constant crying) and appeared reflux/allergic.
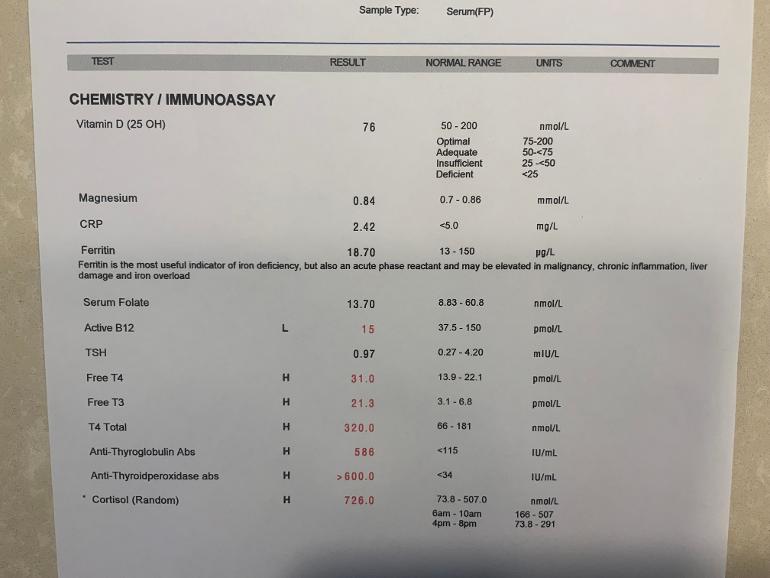
Her results suggest she has an issue digesting/processing certain things as despite eating a very healthy and varied organic diet with lots of meat/fish/eggs, her active B12 is on the floor and her ferritin has been dropping off. She has always taken a multivitamin as well with both these things in. She was only off this for two weeks before this test. The NHS has tested her B12 in the past but this was always total B12 only and this number has always been high in range, I never thought to question it. It is only by chance I tested my thyroid recently with an active B12 test in it and discovered it to be low that I realised hers has never been tested and wondered if she had issues with this as well.
Anyway, it looks like she needs B12 injections to boost her but I’m wondering about whether there is a general digestion issue at play (given low ferritin too) and also what is going on with her thyroid…? The last thyroid test had mildly elevated antibodies but these are through the roof but her FT4/FT3 are ridiculously high also. Cortisol also too high, again! At the time of the test we tried to do a FBC but those bloods didn’t arrive at the lab stable so they couldn’t do them. We know our daughter was suffering from low platelets at the time as she had several large unexplained bruises on her leg (one like a hematoma) and a “cold”.
Anyone with any advice or similar experiences, it will be gratefully received! Thank you!