hello, I have been feeling pretty unwell with a variety of symptoms for about a year. I’ve had a few different tests and procedures and nothing that really explains any of my symptoms has been found. When googling a lot of my symptoms sounded similar to what I read to hypothyroidism so I paid privately for a more in depth test than my gp had done and my thyroid antibodies have come back high - my thyroglobulin was 310 ku/l (lab range is 0-115) and thyroid peroxidase was 359 Kiu/l (lab range 0-34) My TSH was 2.93 mil/L, FT4 was 14.2 pmol and FT3 was 4.6 pmol. I have arranged an appointment with my GP but it’s a telephone call over a week away and I’m feeling quite unwell. Could this be the reason? Thank you in advance for reading and for any advice
thyroid antibody test : hello, I have been... - Thyroid UK
thyroid antibody test
Welcome to the group. If you could complete your profile it helps members understand your thyroid journey so far and be able to advise you better. Click on your image icon to start. Fill out the free text box at the top.
Can you tell us what time of day this test was taken? TSH (needs to be above range) is what often gets people a diagnosis. It runs on a circadian rhythm and is highest at 9am or earlier.
What are the reference ranges for your results? This will be the numbers in brackets after your result number. They are important as labs have different ranges and without them we dont know where your results fall.
Positive thyroid antibodies signify that you have autoimmune thyroid disease sometimes known as Hashimoto's disease. The NHS doesnt really refer to it as that.
Your thyroid is very slowly being destroyed but it can take years before your blood results peep outside of the range so that you can begin treatment.
Ask your GP to test you every 3-4 months to keep an eye on your levels and always book 9am blood test, only drink water that morning and have breakfast after the test for consistency in results.
People with Hashi's can improve symptoms by going strictly gluten free. Some also benefit from removing dairy from their diet.
When hypo we get low stomach acid which means we cannot absorb vitamins well from our food, regardless of a great diet. For thyroid hormone to work well we need OPTIMAL levels of vitamins. Have you recently or could you ask your GP to test levels of ferritin, folate, B12 & D3? Private tests are available, see link for companies offering private blood tests & discount codes, some offer a blood draw service at an extra cost.thyroiduk.org/testing/priva...
There is also a new company offering walk in (includes free blood draw) & mail order blood tests in London, Kent, Sussex & Surrey areas. Check to see if there is a blood test company near you. onedaytests.com/products/ul...
Only do private tests on a Monday or Tuesday to avoid postal delays.
Thank you for replying. I will complete the profile after this reply.
The test was taken about 9.30 am I think (I had fasted from the night before)
TSH range was 0.27 - 10 mil/L (my result 2.93) FT4 range was 0-30 pmol (my result 14.2) FT3 range was 0-10 pmol (my result 4.6) T4 range was 0-300 nmol/L (my result 100)
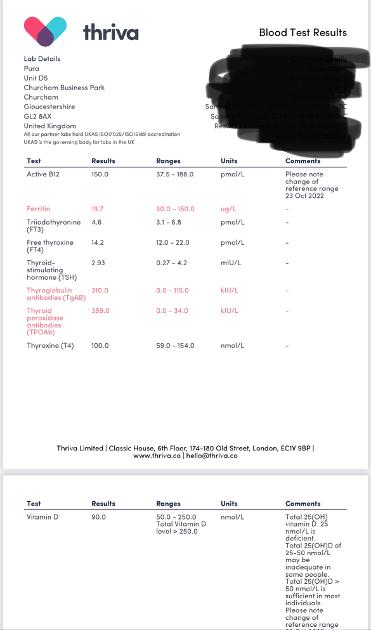
My ferritin, b12 and vit d were all tested at the same time. My iron is chronically low it has been low all year despite supplementing, eating meat, taking supplements with orange juice ect it doesn’t seem to be rising very much. It is currently 19.7 ug/l (lab range 0-400) that is up from 16 ug/ l after supplementing for the last four months from gp. Active b12 is over 150 pmol (I have had 6 injections over 6 weeks in the last couple of months and taken a daily b supplement after a borderline low result in June ) and vitamin d is 90nmol (lab range 0-300) this has gone up after supplements from a borderline low result is august (I stopped all supplements a week before performing the thyroid blood test)
I was lucky my dr requested homocysteine blood test after my borderline low b12 test in June and that came back high (19.4 umol/l) My folate at that point was 6.0 ug/l and hasn’t been tested since
The ranges you have given cannot be correct as they wouldn't start at 0.
Which iron supplements have you been taking?
It can take many many months to raise iron so dont give up. You could try a different supplement if the one you have isnt working. Many members of this group use this product with success. Terrible website but great product.
threearrowsnutra.com/en-uk/...
If you are having B12 injections then its importsnt that cofactors for B12 are also good. This makes your iron even more important along with a few others.
Suggest you start a B complex that would also include folate and help keep all the B's in balance, they need each other to work well.
Slightly cheaper options with inactive B6:
amazon.co.uk/Liposomal-Soft...
Contains B6 as P5P an active form:
bigvits.co.uk/thorne-resear...
healf.com/products/basic-b-...
Explanation about the different forms of B6:
helvella.blogspot.com/p/hel...
B complex comparison spreadsheet:
healthunlocked.com/thyroidu...
A magnesium supplement would also be helpful.
Thank you. I just put 0 for where the line began I obviously have misunderstood the number you asked for sorry.
The iron I take is Ferrous Fumarate 210mg from GP. I will take a look at the one you have recommended thank you.
I do take a b complex (sorry I think I just called it a b supplement in my last post) I do follow b12 society advice regarding cofactors I just do not seem to have had much improvement as yet. I do also take a magnesium supplement (nutrition geeks glycinate 3 in 1 do you know if that one is ok) Thanks so much for your time
Tsh 0.27-10, ft4 12-40, ft3 3.1-10, t4 5.9-15.4 (do they seem more accurate?) sorry I tend to just look and take what is says where my marker falls for my results
It's often helpful to edit your original post when updating for info like this, so we can read it all in context. You can hit the "More" then "Edit" in the dropdown menu.
Thank you for the advice. Someone else has commented the levels seem strange so I’m going to try and upload a picture as I could still be adding incorrect info.
Don't worry. I was curious to see where your FT4 in particular fell. (just seen you have uploaded Thriva results)
Which lab was it MMH?
The main thing is you need 2 NHS tests abive TSH range for diagnosis & to begin treatment.
It can take quite a few months for B12 to take effect plus you need the cofactors including iron which looks like it will take a while too.
On top of that you have on the low side thyroid levels that will be fluctuating so you might need to settle in for the long term keeping an eye on everything.
Well done for taking care of all the cofactors for B12 (and thyroid).
Hi Bruce
Welcome to the forum
Have to say, these seem very unusual ranges 🤔 (where marker falls🤔 GlowCoach )
Are you able to perhaps anonymise your results and take a photograph and post here using the picture button at the bottom of the reply box (next to smiley face). Formats differ so sometimes it is just easier to see what you have been given. Where about are you anyway (no specifics ), Just region - we need to maintain your privacy 🤗
Request GP do ultrasound scan of thyroid
Also coeliac blood test as per NICE guidelines
nice.org.uk/guidance/ng20/c...
1.1 Recognition of coeliac disease
1.1.1 Offer serological testing for coeliac disease to:
people with any of the following:
persistent unexplained abdominal or gastrointestinal symptoms
faltering growth
prolonged fatigue
unexpected weight loss
severe or persistent mouth ulcers
unexplained iron, vitamin B12 or folate deficiency
type 1 diabetes, at diagnosis
autoimmune thyroid disease, at diagnosis
irritable bowel syndrome (in adults)
first‑degree relatives of people with coeliac disease.
Thank you for taking the time to comment and for the advice. I have had a celiac blood test when my symptoms began. It came back mildly positive and I was sent for an endoscopy, there was no eveidence of disease and biopsies were taken which came back clear so I’m pretty sure I can say that has been checked thoroughly? Gluten intolerance could definitely be a cause though as I do eat gluten containing products so I will try cutting it out and see if it helps anything. At the time of the positive test I saw one gp who told me the blood test meant I definitely had celiac disease and another that said other things can cause the blood test to be positive but once celiac was ruled out nothing else was ever investigated so I’ve no idea what those other things are or if it is the same as these that have come back raised now. I shall have to mention it at the upcoming appointment.
Your antibodies are high this is Hashimoto's, (also known by medics here in UK more commonly as autoimmune thyroid disease).
Hashimoto's affects the gut and leads to low stomach acid and then low vitamin levels
Low vitamin levels affect Thyroid hormone working
Poor gut function can lead leaky gut (literally holes in gut wall) this can cause food intolerances.
Most common by far is gluten.
Dairy is second most common.
A trial of strictly gluten free diet is always worth doing
Only 5% of Hashimoto’s patients test positive for coeliac but a further 81% of Hashimoto’s patients who try gluten free diet find noticeable or significant improvement or find it’s essential
A strictly gluten free diet helps or is essential due to gluten intolerance (no test available) or due to leaky gut and gluten causing molecular mimicry (see Amy Myers link)
Changing to a strictly gluten free diet may help reduce symptoms, help gut heal and may slowly lower TPO antibodies
While still eating high gluten diet ask GP for coeliac blood test first or buy test online for under £20, just to rule it out first
Assuming test is negative you can immediately go on strictly gluten free diet
(If test is positive you will need to remain on high gluten diet until endoscopy, maximum 6 weeks wait officially)
Trying gluten free diet for 3-6 months. If no noticeable improvement then reintroduce gluten and see if symptoms get worse
chriskresser.com/the-gluten...
amymyersmd.com/2018/04/3-re...
thyroidpharmacist.com/artic...
drknews.com/changing-your-d...
Non Coeliac Gluten sensitivity (NCGS) and autoimmune disease
pubmed.ncbi.nlm.nih.gov/296...
The predominance of Hashimoto thyroiditis represents an interesting finding, since it has been indirectly confirmed by an Italian study, showing that autoimmune thyroid disease is a risk factor for the evolution towards NCGS in a group of patients with minimal duodenal inflammation. On these bases, an autoimmune stigma in NCGS is strongly supported
nuclmed.gr/wp/wp-content/up...
In summary, whereas it is not yet clear whether a gluten free diet can prevent autoimmune diseases, it is worth mentioning that HT patients with or without CD benefit from a diet low in gluten as far as the progression and the potential disease complications are concerned
restartmed.com/hashimotos-g...
Despite the fact that 5-10% of patients have Celiac disease, in my experience and in the experience of many other physicians, at least 80% + of patients with Hashimoto's who go gluten-free notice a reduction in their symptoms almost immediately.
Similarly few months later consider trying dairy free too. Approx 50-60% find dairy free beneficial
With loads of vegan dairy alternatives these days it’s not as difficult as in the past
Post discussing gluten
With ferritin that low you need to ask for a full iron panel to get a complete picture. You nay need an infusion as oral supplementation isn't helping much. Folate's low and you need to get levels up, especially if injecting B12.