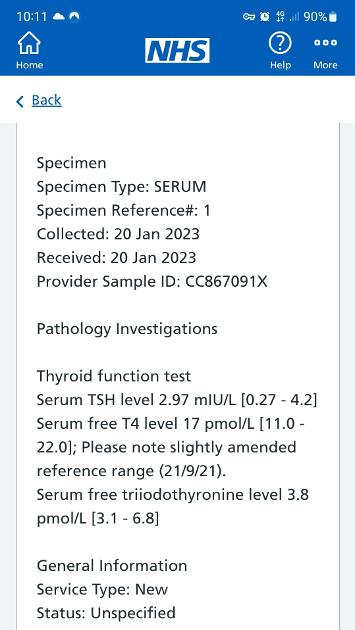
T4/T3 conversion Doctor has put on notes normal no further action even though I'm on 100mg Levothyroxyine weight 15st and symptomatic
Recent blood test, is it necessary to have RT3 ... - Thyroid UK
Recent blood test, is it necessary to have RT3 test done if ratio T4/T3 is low?
You have a T4/T3 conversion doctor on the NHS? Amazing they did your FT3!
Your FT3 level is only at 19% so you really need a dose increase of 25mcgs.
RT3 test is not so popular these days as there are many many causes of high RT3.
I would say you are symptomatic because your TSH is too high. It should be 1 or less when being treated. There is room for an increase in Levo. This may also bring up your FT3 which will help with your symptoms.
Some members will come along and give links to guidelines that you can show your GP. You will have to be your own advocate.
Previous T4/T3 conversion
No you don't need rT3 done , its very expensive and even if it's high there can be a multitude of reasons for it ... if the cause is 'too high T4' you can see that by looking at fT4 / fT3 tests .
Time of day affects TSH result , early am highest >>> early / mid afternoon lowest .
Those TSH results from Oct / Dec 2021 were done when it was lowest .. if done at 9/10 am they would have been higher.
.....What time of day was this latest TSH result of 2.97 taken ?
Show your GP this list of recommendations advising GP's to keep TSH below about 2/2.5 in patient taking Levo ( some written specifically for GP's by NHS registrars in Cardiology and Endocrinology) healthunlocked.com/thyroidu... my-list-of-references-recommending-gp-s-keep-tsh-lower
and use it to ask for a trial increase in Levo dose to 112.5mcg or 125mcg for 6 months .. to see if it improves your remaining symptoms .
How long have you been on propranolol
On all these tests?
Breathlessness is frequently low iron/ferritin
Get full iron panel test for anaemia including ferritin
Always do iron test early morning, and just water before test and don’t eat iron rich dinner night before test.
Medichecks iron panel test
medichecks.com/products/iro...
also need to test BOTH TPO and Tg thyroid antibodies privately
Stace268
is it necessary to have RT3 test done if ratio T4/T3 is low?
No. There are many reasons for raised rT3 and only one of them is connected to the thyroid. Testing can tell you if it's high but can't tell you why so it's a pointless test that's not worth spending money on.
An excess of unconverted T4 can cause high rT3, your FT4 is too low for this to cause high rT3. The other conditions that contribute to increased Reverse T3 levels include:
· Chronic fatigue
· Acute illness and injury
· Chronic disease
· Increased cortisol (stress)
· Low cortisol (adrenal fatigue)
· Low iron
· Lyme disease
· Chronic inflammation
Also selenium deficiency, excess physical, mental and environmental stresses. Also Beta-blocker long-term use such as propranolol, metoprolol, etc. Physical injury is a common cause of increased RT3, also illnesses like the flu. Starvation/severe calorie restriction is known to raise RT3. Diabetes when poorly treated is known to increase RT3. Cirrhosis of the liver. Fatty liver disease. Any other liver stress Renal Failure. A fever of unknown cause. Detoxing of high heavy metals.
Articles
thyroidpatients.ca/2019/01/...
zrtlab.com/blog/archive/rev...
verywellhealth.com/reverse-...
Your results clearly show that you are undermedicated to have a TSH level of 2.97, an FT4 that is only 54.55% through range and an FT3 that is 18.92% through range.
The aim of a treated hypo patient on Levo only, generally, is for TSH to be 1 or below with FT4 and FT3 in the upper parts of their reference ranges.
Did you do the test as we advise:
* No later than 9am
* Water only before the test
* Last dose of Levo 24 hours before test
* No biotin, B Complex or any supplement containing biotin for 3-7 days before the test
If so then your results suggest that you need an increase in your Levo, 25mcg now, retest in 6-8 weeks, possibly followed by a further increase until levels are where the need to be for you to feel well.
Are your Vit D, B12, Folate and Ferritin at optimal levels, this is needed for thyroid hormone to work properly and good conversion to take place. If not tested then it would be a good idea to do this now.
Test was 9:30am and I had a coffee, I had stopped Biotin and vits OK, selenium is non existent though as had this condition since birth.
Stace
We always suggest no food or drink except water before thyroid tests so that nothing interferes with the results.
Coffee is said to interfere with blood test results
healthline.com/health/fasti...
Can you drink coffee if you’re fasting before a blood test?
Even if you drink it black, coffee can interfere with blood test results. That’s because it contains caffeine and soluble plant matter, which might skew your test results.
selenium is non existent though
Have you tested and know that your level is non-existent? Are you supplementing? Selenium is important for thyroid function.
"selenium is non existent though as had this condition since birth."
"Selenium came up as 0 when I had it tested because I thought I had thyroid eye disease"
What condition have you had since birth ?
have you had low / '0' tests for selenium previously ?
Selenium is a vital part of the process for thyroid hormone production AND for conversion of T4 >> T3. without it the deiodinases (DIO1/ DIO2 ) will probably struggle to convert T4>>T3 properly
(i say probably because . selenium together with iodine play a very complex role in this process and most of it is 'over my head' )
Do you supplement with selenium ?
Hello Stace :
I'm not aware the NHS test or recognise Reverse T3 - and they are not obliged to accept private blood test results and they refused to accept my complete thyroid blood tests to include a Reverse T3 some 6 years ago.
In order for T4 monotherapy to work effectively we do need to maintain optimal levels of ferritin, folate, B12 and vitamin D :
Once these vitamins and minerals are at good levels and your core strength strong and solid you will be better placed to build up our dose of T4 into the top quadrant of the range as then the conversion to T3 - the active hormone - should improve to around 60/70% through it's range.
The accepted conversion ratio when on T4 monotherapy is said to be : 1 - 3.50-4.50 - T3/ T4 with most people feeling at their best when they come in this ratio at 4 or under.
We generally feel better when the TSH is low in the range and definitely under 2 and more probably under 1 and this will happen with slow steady increase in T4 - Levothyroxine at 25mcg increments and a blood test follow ups every 6- 8 weeks to follow your progress and hopefully to the relief of symptoms.
The conversion ratio doesn't really apply at this point in time as your T4 is not in the top quadrant and when there are insufficient thyroid hormones circulating the body prioritises T3 over T4 so your current conversion ratio 17 divided by 3.80 - is not a true reflection of your ability to convert T4 into T3.
Do you have any recent vitamin and mineral blood test results as forum members can advise of where these need to be as some of the NHS ranges are too wide to be serious.
Vitamins fine
Vitamins ok
I can't see a ferritin ?
OK just for reference I know now that I need to maintain my vitamins and minerals at the following levels to feel well and able to convert T4 into T3 :
I need a ferritin at around 100 : folate at around 20: " serum " B12 at 500 ++ and a vitamin D at around 100:
Folate not Ferritin?
suggest you change vitamin D supplement
Vitamin D mouth spray by Better You is very effective as it avoids poor gut function.
There’s a version made that also contains vitamin K2 Mk7.
One spray = 1000iu
amazon.co.uk/BetterYou-Dlux...
Increase to 2000iu and retest in 3-4 months
Test twice yearly via NHS private testing service when supplementing
Aiming for at least over 80nmol and between 100-125nmol may be better
My doctor prescribes the Vitamin D and I know I have low stomach acid so it's very probable I have absorption issues. Though it was at 25mg at one point and now 69 so it must be working slowly. GP also told me too much calcium is bad for heart, I believe she's trying tell me something.
Oh dear another clueless medic!!
You need to optimise vit D, vit B12, folate and ferritin to support T4 to T3 conversion/ thyroid function....it will take a littlt time to raise levels so be patient
Low essential nutrients impair conversion
Poor conversion can be identified simply .....high FT4 with low FT3
Your levels are going in that direction....but this can be reversed with corect treatment
T3 is the active thyroid hormone and for good health must be available in an adequate and constant supply
Low cellular T3 = poor health
Your FT3 level is abysmal!
FT3 followed by FT3 are the important readings....TSH is not a reliable marker....see link below.
100mcg levo is not providing the hormone level you need and I suspect your nutrient levels are low
Weight gain is a symptom of hypothyroidism/ undermedication
First you need to raise levo to 125mcg along with any deficient nutrients ( above) then after 6/8 weeks on a steady dose test again.
You still have plenty room to raise levo to 150mcg if FT3 is still too low......both FT4 and FT3 should be approaching 75 % through the ref range...we are all different so this will vary.
Listen to your body it will tell you when treatment is working....or not
If that does not adequately raise FT3 and improve symptoms then you may need to add a little T3....but you are not at that point yet
Your GP will most likely wrongly focus on TSH and bang on about overmedication because your TSH has fallen....rubbish!
This link will explain and help argue your case if TSH becomes an issue with your medics
thyroidpatients.ca/2021/07/...
As for rT3....it is basically the body's way of getting rid of excess T4....it can rise when FT4 is not being adequately converted but it is transient and is fairly quickly metabolised and excreted. Expect rT3 to be low if FT4 is low. Don't worry about it....correct medication will resolve this. Testing is expensive and not needed!
The NHS report above is wrong to say no further action needed....initially you need more levothyroxine
"Normal" only means in ref range. it does not mean that your results are optimal for you as an individual....it is a pointless term
Just a few thoughts!
I know this but how can you make a doctor retest in 6-8 weeks to get results if they refuse and refuse increase
"how can you make a doctor retest in 6-8 weeks to get results if they refuse and refuse increase"
re. what to do it they refuse an increase when bloods clearly say there is room to try one safely ?
.. personally i "do it first and ask later" ..
eg i increase dose slightly myself for at least 6 weeks using the tablets i already have ( if i didn't have enough in hand to do 6 weeks i might accidentally 'leave a packet on holiday and request a 'replacement' doing this once will not be a problem . obviously it's not a way to get more long term)
increase by 12.5mcg (or 25mcg but no more) for at least 6 weeks (just before the next GP 'annual' blood test is due if possible, as then you don't even have to explain why you want 'another' blood test .... but if that is too far away just do it for 6 weeks whenever , and then say "i've tried increasing my dose and i feel better, can we check my bloods on it please" .. they will have to agree to do bloods then because they will be worried you are overmedicated )
Then book test and tell phlebotomist you have recently been trying an increase to 'x' so it's officially noted and GP will be informed of what you've done .
Then book appointment to "discuss result with GP" .. assuming the TSH is still in range and the fT4 is not over range .. the GP will have no legitimate grounds to ask you reduce again . and should be willing to increase the prescription officially to 'x'
obviously if the TSH is now below range and /or fT4 is over range , then you will be having a different conversation .. hence why it is better to only increase by 12.5mcg at a time..as it reduces the chances of the GP having a dicky fit
( it's a good idea anyway regardless of the GP's stress levels ... 12.5mcg IS enough to have an impact on symptoms .. and we don't want to be taking more than we need ....12.5mcg 'too much' can make you feel just as rubbish as 12.5mcg 'too little'
20 yrs ago i increased my own dose from 50 to 100 to 150 using this method .. (because i didn't know any better) . My TSH was in range each time and fT4 was not over range , so GP always said "ok ,carry on" ,
I would be more cautious nowadays and would have gone from 100 to 125 to 137.5.. as i've since learned that 12..5 mcg is enough to make a difference to symptoms , and i've also experienced overmedication (which is actually quite hard to spot when it come on gradually over several months) but is very unpleasant.
That all makes sense to me, though I was just going to mention the GP handbook on Thyroxine and I felt better when it was 1.44 in 2021 also I'm concerned of damage being under medicated. On a different note I read of someone has conversion issues too high T4 can be damaging as they pituitary can't convert it. Feel lost tbh and over and undermedicated are similar so you're right, though as with you unlikely I'm over.
pituitary doesn't really do 'converting' T4>>T3 .. (well every cell/ organ that has any thyroid hormone receptors must be capable of converting 'some' ... but conversion of T4 to T3 is a whole body thing involving lots of different organs and cells .. not so much a 'pituitary' thing .. if you see what i mean ) ~ edit * if you can you give a link to what you read i can maybe try and help understand what you read .
Anyway ... i really don't think you do currently have any issues with 'too high' T4
FT4: 17 pmol/l (Range 11 - 22) 54.55% ( thyroid.dopiaza.org/ % calculator)
if fT4 was 90% or 125% when fT3 was 18% ,that would be different ... but currently your fT4 is not even as high as high as many healthy people with no thyroid issue would have. Your fT3 will likely increase as your fT4 increases on higher dose .. if it doesn't and you have improved vitamins etc to optimal if needed .. then that is the time to start thinking about conversion .. and whether to investigate lower Levo with added T3.
P.s what's the issue with your selenium ? is it really "Zilch " or has it always been just low ? do you know why ?
Do you know selenium is an absolutely VITAL part of the (chemical /cellular /deiodinase ?) process of thyroid hormone production AND conversion ?
It's effects on thyroid hormone production and conversion are complex and mostly 'over my head' ..and Selenium interacts in a very complex way with iodine levels too .. (iodine is a whole other area that needs MUCH CAUTION as it also has a direct effect on thyroid function , and too much can cause just as many problems as too little.)
OK. Well, knowing is a good start...you have to use that knowledge to your advantage and beat them at their own game....many of us have had to do this....see Tatty's response as an example
Your post didn't say your GP was refusing to budge...you appeared to be asking about rT3 and conversion....hence my response. We need as much relevant info as possible to be able to help
Take control ...raise your levo dose yourself... you have plenty room to do this safely. If you feel better use that to convince the GP you need an increase...if he objects then ask him to explain what else could have caused improvement....bet he struggles!
You will not be overmedicated so long as FT3 is in range
Test privately....basic tests won't break the bank and will point the way forward
See another GP who may be more switched on
Speak to the Practice Manager and say you feel very unwell but your GP isn't listening to you and taking your symptoms into consideration....result you are undermedicated and unwell and your labs prove this
Raise the point about the importance of adequate T3....you say you know all about that so use that knowledge.
The GP is most likely struggling due to lack of knowledge and can only trot out the usual TSH drivel
As an aide memoir before an appointment make a list of all the points you want to raise so that you can have a well informed discussion with the GP.....and hope he is open minded.
Refer to the link I posted and use this Paper too , for ref..
bmcendocrdisord.biomedcentr...
Time for a reassessment of the treatment of hypothyroidism
John E. M. Midgley, Anthony D. Toft, Rolf Larisch, Johannes W. Dietrich & Rudolf Hoermann
The authors are eminent in the field and cannot be dismissed....including TUK's advisor, diogenes, who is first author.
They will quickly knock you back if you just request an increase....prove to them that you need it.
I think mine is a Dio1 gene issue, and did you see past T4/T3 results back in 2021 I posted picture. Selenium came up as 0 when I had it tested because I thought I had thyroid eye disease
We try to, but I'm afraid we don't always have time to trawl through old posts so try and add relevant info in any queries you raise, with linksif possible....it helps us to help you.
I suspect you are overthinking some of this....suggest you concentrate on getting your levo levo increased which should help.
It's easy to feel overwhelmed if you try to sort out everything in " a lump". Tackle one thing at a time
I also suspect your Vit D is deficient...
The Vit D Council, recommends a level of 100-150nmol/L (40-60ng/ml),.. is your level within this parameter
Re selenium...Protein foods from animals are generally good sources of selenium. Seafood, organ meats, and Brazil nuts are the foods highest in selenium followed by everyday stap like breads, cereals, poultry, red meat, and eggs.
Selenium deficiency is rare worldwide, and it often takes years to develop. It usually only occurs in regions with severely low selenium content in the soil, Are you sure your result was zero?
Re Dio1 and Dio2 snps....we have already discussed this...see previous posts. You cannot alter your genetic make up but you can deal with the possible consequences of identified polymorphisms eg impaired T4 to T3 conversion by adjusting medication.
First, you need more levothyroxine as we have previously explained.
The picture aforementioned is within this post not an old one.Yes pretty sure it was 0 and like I said it's been present since birth so it's possible though not had it tested recently only few years ago.
I will and do want to concentrate on T4 increase though I think because of already developed heart disease and just GP awkwardness they're being difficult.
Yes vit now 69 (was 23) as shown in this post also.
Many thanks
just curious .... why were they testing selenium at birth ? does it relate to a particular health condition/ diagnosis .. or just a random "this kid has no selenium, but we don't know why "...please feel free to not answer this question if you don't want to ... like i said i'm just curious.
They didn't test at birth I recall a conversation with a GP now left the practice who tried convince me go on Levothyroxine at in my twenties and she warned me about long untreated hypothyroidism and can cause a deficit in Selenium amd how it affects the eyes or in pregnancy. Some time later in my thirties after pregnancy I had it tested and it was zero
There is a result below the serum B12 readings :
Sorry I meant to say GP did not test Ferritin
Oh !! I've only found this last message from you by accident - i think we have problems with Ground Control :
Ok - obviously we need to see where your ferritin is as it's very common when hypothyroid to be low - mine was 22 - and we need a ferritin of at least 70 for any thyroid hormone replacement to work well - or so I read - and I now aim for around 100 :
Hi, I'm on the UK NHS I can't see my GP willing to test it?
Oh I know it's hopeless -
I gave up around 6 years ago and run a yearly full thyroid panel and the vitamins and minerals for myself as I need to keep supplementing even though I'm now optimally medicated.
That’s why there’s over 120,000 members on here
Vast majority are based in U.K.
Thousands upon thousands test privately to make progress and as annual self review to maintain OPTIMAL vitamin levels and test TSH, Ft4 and Ft3 (plus helpful to check how fast antibodies are reducing if on gluten free/dairy free diet)
You need full iron panel test for anaemia including ferritin
Vitamin D better at least over 80nmol and between 100-125nmol may be better
How much vitamin D are you currently taking
Are you supplementing magnesium too (in afternoon or evening at least 4 hours away from levothyroxine)
800iug vit D3 plus normal amount in a multivitamin which includes magnesium in it. I've read and heard too much magnesium is bad for heart and drinking water has magnesium in, Yes take vitamins 4hrs apart from it. Not concerned about Iron panel, I said it was when I was a kid I had anemia and I never know what to ask for the GP does not really keep eye on anything even if specialist sends a letter I have to chase it up as they don't bother reading it.
Never take iron supplements without getting full iron panel test
Multivitamins never recommended on here. Most contain cheap poorly absorbed ingredients and also anyone on levothyroxine doesn’t want extra iodine. Levothyroxine contains all the iodine you need
Suggest get a separate selenium supplement
And retest selenium levels in 6 months
Guidelines on dose levothyroxine by weight is that most people eventually need approx 1.6mcg Levo per kilo of their weight
15st = 95kg
95kg x 1.6mcg = 152mcg as the likely daily dose levothyroxine you might require
We ONLY increase dose by 25mcg a day
Get dose increase to 125mcg
Make sure both tablets are always same make
Which brand are you currently taking
Always Take levothyroxine on empty stomach and then nothing apart from water for at least an hour after
I forgot to say I take a separate methylated vitamin B complex and what does everyone else take in regards multivitamin do they use methylated? It's so expensive!
I do space everything out as im on propranolol and spironolactone but trying stop the propranolol completely as hinders conversion apparently.
Yes only take with water and leave for an hour.
I am take Mercury Pharma brand.
Test folate, B12 and ferritin at least once a year
Test vitamin D (ideally) twice year
Supplement only what tests show you need
Typically that’s daily vitamin D, daily vitamin B complex (one with methyl folate) and daily magnesium
Magnesium best taken afternoon or evening, but must be four hours away from levothyroxine
Vitamin D…..dose required varies a lot between individual people
Likely to need higher dose if gluten free or malabsorption
Aiming for at least over 80nmol and between 100-125nmol might be better
Daily vitamin B complex should keep all B vitamins in balance and folate and B12 optimal
If vegetarian/vegan or malabsorption issues might need separate B12 supplement a few days a week
Similarly ferritin needs testing annually. If under 50 need full iron panel to see if iron also low. Aiming for ferritin at least over 70, nearer 100 better. If iron is good, can’t take iron supplements. Would need to improve ferritin just by increasing iron rich foods in diet
I thought if Folate high enough Ferritin should be OK?
Also what's active B12, most GP only test normal B12.
Also worried about taking magnesium too regularly if affects heart, I do get sharp pain in my left foot feels like nerve pain every so often.
Ferritin is storage form of iron
Nothing to do with B vitamins
Medichecks tests Active B12
NHS and Blue Horizon test serum B12
Magnesium is good for your heart
Modern soils are low in magnesium
So vegetables and diet is frequently low in magnesium
Magnesium best taken in the afternoon or evening, but must be four hours away from levothyroxine
betterbones.com/bone-nutrit...
medicalnewstoday.com/articl...
livescience.com/61866-magne...
sciencedaily.com/releases/2...
Interesting article by Dr Malcolm Kendrick on magnesium
drmalcolmkendrick.org/categ...
Vitamin K2 mk7
betterbones.com/bone-nutrit...
healthline.com/nutrition/vi...
2 good videos on magnesium
healthunlocked.com/thyroidu...
I know B vitamins are nothing do with Iron. It was separate.My dad's on Wafrin and Vitamin K lowers his Wafrin.
My MCH has quite often been over range so now I wonder if my hypothyroidism is primary or secondary.
That’s different K vitamin with warfarin (k1)
K2 mk7 helps direct calcium to bones to restore strength
High MCH
Low vitamins are extremely common when hypothyroid as we frequently develop low stomach acid, leads to poor nutrient absorption and low vitamin levels as direct result
healthline.com/health/mch#t...
Treatment for anemias caused by B-12 or folate deficiencies are commonly treated by lifestyle changes, such as adding foods rich in vitamin B-12 and folate to your diet. Your doctor may also recommend taking supplements of these vitamins to further boost your B-12 and folate levels
If GP won’t test iron and ferritin
Medichecks iron panel test
medichecks.com/products/iro...
Good point regarding the Vit K I forgot about that! Thanks.
In 2020 Ferritin was 65. I really can't afford keep paying for these tests and tbh I feel my GP or specialist should be keeping an eye on me that's what they're paid for.
NHS only tests and treats vitamin deficiencies
Not obligated to maintain optimal vitamin levels
That’s down to us to do
NHS is not interested in managing hypothyroid patients correctly
They don’t understand the interconnected between low vitamin levels and poor conversion
Your obviously on too low a dose levothyroxine for your weight
And propranolol is badly affecting conversion and uptake of Ft4 to Ft3
Why was propranolol prescribed originally
Anxiety and I told her that I'm getting a lot of pains in my chest. Funnily low T3 can cause that.
Echo scan shows borderline Right sided hypertrophy.
My dad has heart failure.
My grandad had a stent put in after strokes.
My son has autism and multiple learning difficulties.
Hoping no connection to my health.
Anxiety is extremely common hypothyroid symptom
Also gluten intolerance extremely common with autoimmune thyroid disease (hashimoto’s)
Gluten intolerance can cause anxiety
Presumably you have Hashimoto’s
I was stuck on propranolol almost 20 years (anxiety)
Going gluten free was astonishing. Finally got off propranolol. More on my profile
If you have high thyroid antibodies (hashimoto’s) GP should test for coeliac BEFORE considering trial on strictly gluten free diet
Approx 86% of Hashimoto’s patients who try strictly gluten free diet see noticeable or significant improvement or find it’s absolutely essential
Of that 86% only 5% test positive for coeliac disease
Get your son FULL thyroid and vitamin testing via his GP, including thyroid antibodies
Make sure test is early morning around 9am
autismparentingmagazine.com...
I'm not coeliac and not hashimotos as TP0 negative Again GP not interested apparently they don't treat hypothyroidism in children, sons TSH is borderline like mine.
I am trying cut out high carbs, sugar and wheat just for weight loss more than anything else. Bit like Keto diet
just testing TPO antibodies is inadequate
There’s 2 antibodies implicated in Hashimoto’s
TPO and Thyroglobulin antibodies
NHS refuses to test TG antibodies if TPO antibodies are negative
Significant minority of Hashimoto’s patients only have high TG antibodies
If you test via Medichecks and both antibodies are negative
20% of Hashimoto's patients never have raised antibodies
healthunlocked.com/thyroidu...
Paul Robson on atrophied thyroid - especially if no TPO antibodies
paulrobinsonthyroid.com/cou...
I've been diagnosed with hypothyroidism is TG antibodies important?I had Dio2 test said I have wild type TT genotype.
I think I carry MTHR gene but scared to test it.
You won’t make progress on thyroid levels until completely off propranolol
Are you slowly reducing dose
How much are you currently taking per day
Then once all vitamins are optimal you might get T3 prescribed
I am heterozygous Dio2 (inherited from one parent)
It probably helped get T3 prescribed on NHS
But couldn’t tolerate T3 or improve vitamin levels until off propranolol and on strictly gluten free diet
More on my profile
I'm only on 10mg(sorry got it wrong) today was alternative day but I didn't take it.I've read beta blockers are listed as life saving drug but it I can do without it and no chest pains I'd be better off.
Gluten is in wheat, barley and rye
Gluten free has to be strictly gluten free to be effective
Read all labels carefully
Don’t cut all carbs ….as this reduces conversion rate of Ft4 to Ft3
Just cut beige carbs ….cakes, potatoes, rice, pasta etc
Carbs in veg and fruit are good
How high is your sons TSH
Essential to get his vitamins tested
Ask for referral to endocrinologist for him
Email Thyroid U.K. for list of thyroid specialist endocrinologists and doctors
Some are nhs
tukadmin@thyroiduk.org
Borderline like mine so 4.7 for instance but he symptomatic.
That’s not borderline, that’s hypothyroid
Graph showing median TSH in healthy population is 1-1.5
web.archive.org/web/2004060...
If he has low vitamin levels, this tends to lower TSH
Essential to get vitamins tested and optimal by supplementing if necessary
Autistic children often picky eaters and therefore frequently have low vitamin levels
It was just above range I used mine as comparison. He had two seizures as a baby so worried about side effects of any medication.
How old is he
Would need paediatric endocrinologist specialist in thyroid …..might be like looking for needle in haystack
Can you get his autism consultant to organise vitamin testing if GP won’t
yes propranolol significantly affects conversion and uptake of Ft4 (levothyroxine) to Ft3
Propranolol and thyroid hormone
pubmed.ncbi.nlm.nih.gov/168...
rejuvagencenter.com/hypothy...
labtestsonline.org.uk/tests...
Drugs that may decrease PTH include cimetidine and propranolol.
particularly important to take magnesium supplement if stuck on propranolol
It’s important to only reduce dose propranolol VERY SLOWLY
How much are you currently taking
I was stuck on propranolol almost 20 years. More on my profile
Slowdragon . i found this on "Spironolactone" ....don't know what to make of it ,or even if it matters so i'll just stick it here anyway incase it's useful anyone :
"Pituitary-thyroid function in spironolactone treated hypertensive women"
pubmed.ncbi.nlm.nih.gov/107...
"Abstract
Four weeks high dose spironolactone treatment (Aldactone Searle, 100 mg q. i. d.) significantly enhanced the TSH and T3 responses to an intravenous TRH/LH-RH bolus injection in 6 eumenorrhoeic euthyroid hypertensive women, without affecting basal serum TSH, T3 or T4 levels or the basal and stimulated LH, FSH and prolactin values .... Spironolactone, possibly by virtue of its antiandrogenic action, may exert its enhancing effect on pituitary-thyroid function by modulating the levels of receptors for TRH in the thyrotrophs or by altering the T3 receptor in the pituitary permitting a greater response to TRH."
That’s Igennus vitamin B complex
Probably only need one per day. After breakfast
I find this is best vitamin B complex for me
I like these ones too, usually only take 1 unless really tired.
I take them 4 hrs after propranolol and Spironolactone.
How much propranolol are you currently taking
Clear guidelines on dose levothyroxine by weight
pathlabs.rlbuht.nhs.uk/tft_...
Guiding Treatment with Thyroxine:
In the majority of patients 50-100 μg thyroxine can be used as the starting dose. Alterations in dose are achieved by using 25-50 μg increments and adequacy of the new dose can be confirmed by repeat measurement of TSH after 2-3 months.
The majority of patients will be clinically euthyroid with a ‘normal’ TSH and having thyroxine replacement in the range 75-150 μg/day (1.6ug/Kg on average).
The recommended approach is to titrate thyroxine therapy against the TSH concentration whilst assessing clinical well-being. The target is a serum TSH within the reference range.
……The primary target of thyroxine replacement therapy is to make the patient feel well and to achieve a serum TSH that is within the reference range. The corresponding FT4 will be within or slightly above its reference range.
The minimum period to achieve stable concentrations after a change in dose of thyroxine is two months and thyroid function tests should not normally be requested before this period has elapsed.
Ferritin level in 2020
obviously that’s 2…..almost 3 years old
Retest annually
I probably am going into menopause as well, is there a test that covers everything and I'll do it once a year.
Test both TPO and TG antibodies at least once
List of private testing options and money off codes
thyroiduk.org/getting-a-dia...
usually cheapest including antibodies
Medichecks Thyroid plus antibodies and vitamins
medichecks.com/products/adv...
Blue Horizon Thyroid Premium Gold includes antibodies, cortisol and vitamins
bluehorizonbloodtests.co.uk...
Monitor My Health also now offer thyroid and vitamin testing, plus cholesterol and HBA1C for £65
(Doesn’t include thyroid antibodies)
monitormyhealth.org.uk/full...
10% off code here
thyroiduk.org/getting-a-dia...
if testing vitamin D twice year
Use this for second test
NHS easy postal kit vitamin D test £29 via
Only do private testing early Monday or Tuesday morning.
Watch out for postal strikes, probably want to pay for guaranteed 24 hours delivery
I have high cholesterol and spontaneous high Cortisol they suspect Cushings but I do not believe that.
High cholesterol directly linked to still being under medicated for thyroid
Your weight suggests you need at least 125mcg - 150mcg levothyroxine per day
nhs.uk/conditions/statins/c...
If you have an underactive thyroid (hypothyroidism), treatment may be delayed until this problem is treated. This is because having an underactive thyroid can lead to an increased cholesterol level, and treating hypothyroidism may cause your cholesterol level to decrease, without the need for statins. Statins are also more likely to cause muscle damage in people with an underactive thyroid.
similarly high cortisol is extremely common when under medicated/poor conversion as adrenals try to compensate for lack of thyroid hormone
As Ft3 levels increase, cortisol levels will reduce