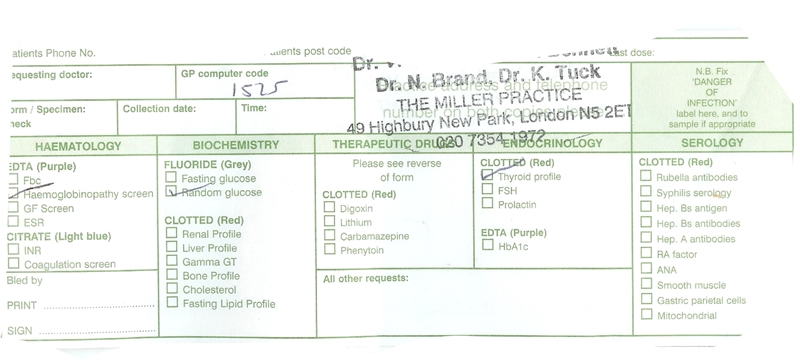
For tests on thyroid antibodies; iron; ferritin; folate; b12 and tests to rule out pernicous anaemia which areas should be ticked on the blood request form, or does the doctor just request these tests in the 'all other requests' section?
For tests on thyroid antibodies; iron; ferritin... - Thyroid UK
For tests on thyroid antibodies; iron; ferritin; folate; b12 and tests to rule out pernicous anaemia which areas should be ticked?
Hi reallyfedup123, thank you, they did test the FT4 which was 15.6 pmol/L (12-22) at the same time as the TSH. So basically, I should just list the tests ideally I would like and if GP agrees, rely on her to request in the appropriate way?
Looks like different surgeries have differen forms , Mine comes from his computer printout A4 sheet and there is all the tests for ferretins, B12 , folites etc too. I am due to have mine in 1st week of Jan for all those.
Mine were requested on computer printout form as C, E, Ferr, VitD & BF.
C was Complete Blood Count (also known as FBC).
E is Electrolytes (kidney function)
Ferr is ferritin.
VitD is Vitamin D3.
BF is B12 & Folate.
Recent TFT request via GP only provided TSH, despite TSH of 107.5. TFT via endos in Jnt Thyroid Clinic always gives TSH, FT4 & FT3. Tg is thyrogen, tested every 6 months post ThyCa & used as a cancer marker to check for recurrence.
Hi Clutter, very helpful, thank you. TSH 107.5, no FT4, amazing. What guidance range for the TSH?
0.35-5.5 Id stopped thyroid meds for 4 weeks as side effects were piling up & making me feel so I'll I really wanted to see if it was Levo. I think it was. All side effects, except facial pain, went.
10 days back on T4 and side effects piling up. Palpitations almost constant 4 hours after taking 100mcg & pain in hip joints woke me throughout last night 
Blood test Thurs & see Dr. Tues/Wed if I can get appt. Surgery won't prescribe T3 so shall have to go it alone I expect.
Will see what response I get to telling Dr. I shall stop T4 & will go to A&E for IV levo when I feel critical. Just in case it embarasses surgery into treating ME & not the mythical 'most' who do well on T4.
Hi Clutter, sorry to hear about your symptoms. Something doesn't sound right medication wise. I would think the first thing would be to get as many test results as possible before proceeding. What were your symptoms and blood test results before you started any medication.
PS: an interesting posting from another forum: Your doctor should be testing FT3 as well as FT4. T4 is the storage form of the thyroid hormones, and it must be converted to the active form, T3, before your body can use it. Some of us convert too slowly, so even though FT4 levels are good (or even a bit high in your case), FT3 levels remain low. As long as FT3 is low, you will not feel well. This can be remedied by lowering T4 meds a little and adding a direct source of T3 meds.
Ask your doctor to repeat labs, testing FT3 as well as FT4 and TSH. FT3 often has to be in the upper half to upper third of the range before symptoms are relieved.
My TSH is suppressed <0.1 and was 0.03 in July. FT4 was 17.1 (9-19) and FT3 3.1 (3.2-6.2). Endo dismissed below range FT3 & my complaint that Levo was making me ill & arranged chest xray and ECG and suggested COPD. Man's an arse. Symptoms have been piling on since I started Levo 20 months ago & improved when Levo stopped and was on T3 only pre RAI twice.
Symptoms went when I stopped T4 in Sept & I've just had lung function tests which graph up well and show lung age to be 3 years younger than my chronological age. Its the T4 but nobody's listening. Incredible I can feel 'weller' with TSH 107.5 than on T4.
I had spiralling hyper & hypo symptoms (Hashi) & hemilobectomy to relieve pressure from nodule on windpipe & gullet. Tumour biopsied positive for stage II Hurthle cell carcinoma so completion thyroidectomy was done 3 months later and I was on 60mcg T3 prior to RAI. Two months later, post RAI, I was put on Levo. That's when my problems REALLY started. TSH is suppressed <0.1 and was 0.03. FT4 was 17.1 (9-19) My FT3 has steadily decreased until it was below range in July at 3.1 (3.2-6.2). Endo cared not. He's happy with my thyroid treatment but arranged chest xray which showed over expanded lungs, ECG which showed some arrhythmia & prolonged QT interval, and diagnosed COPD. 3 months after quitting T4 I can breath easily but went for the lung function test last week to be told that my lung age is 3 years younger than my chronological age. I KNOW my problems begin & end with Levo. My GP 'can't' prescribe T3 and admitted he has another patient with T4 issues. I've an endo appt in Feb (not with 'him' this time) & will see whether she'll prescribe T3. If not, I don't see any point in continuing with endos and will self medicate. I'll not worry about bloods, other than thyroglobulin twice a year and my GP surgery can run those.
I had spiralling hyper & hypo symptoms (Hashi) & hemilobectomy to relieve pressure from nodule on windpipe & gullet. Tumour biopsied positive for stage II Hurthle cell carcinoma so completion thyroidectomy was done 3 months later and I was on 60mcg T3 prior to RAI. Two months later, post RAI, I was put on Levo. That's when my problems REALLY started. TSH is suppressed <0.1 and was 0.03. FT4 was 17.1 (9-19) My FT3 has steadily decreased until it was below range in July at 3.1 (3.2-6.2). Endo cared not. He's happy with my thyroid treatment but arranged chest xray which showed over expanded lungs, ECG which showed some arrhythmia & prolonged QT interval, and diagnosed COPD. 3 months after quitting T4 I can breath easily but went for the lung function test last week to be told that my lung age is 3 years younger than my chronological age. I KNOW my problems begin & end with Levo. My GP 'can't' prescribe T3 and admitted he has another patient with T4 issues. I've an endo appt in Feb (not with 'him' this time) & will see whether she'll prescribe T3. If not, I don't see any point in continuing with endos and will self medicate. I'll not worry about bloods, other than thyroglobulin twice a year and my GP surgery can run those.
I don't know what my bloods were prior to surgery but I was overmedicated to suppress TSH. I was not pleased to see FT3 below range in July but endo was 'happy'. Shortness of breath he diagnosed as COPD has totally cleared since I stopped T4 & lung function test last week showed lung age 3 years younger than my chronological age.
GPs are as useless ad a chocolate teapot when you're treated by endos and only too ready to defer.
Endo appt in Feb and will push for T3 otherwise go it alone.
I had spiralling hyper & hypo symptoms (Hashi) & hemilobectomy to relieve pressure from nodule on windpipe & gullet. Tumour biopsied positive for stage II Hurthle cell carcinoma so completion thyroidectomy was done 3 months later and I was on 60mcg T3 prior to RAI.
Two months later, post RAI, I was put on Levo. That's when my problems REALLY started.
TSH is suppressed <0.1 and was 0.03. FT4 was 17.1 (9-19) My FT3 has steadily decreased until it was below range in July at 3.1 (3.2-6.2). Endo cared not. He's happy with my thyroid treatment but arranged chest xray which showed over expanded lungs, ECG which showed some arrhythmia & prolonged QT interval, and diagnosed COPD.
3 months after quitting T4 I can breath easily but went for the lung function test last week to be told that my lung age is 3 years younger than my chronological age.
I KNOW my problems begin & end with Levo. My GP 'can't' prescribe T3 and admitted he has another patient with T4 issues.
I've an endo appt in Feb (not with 'him' this time) & will see whether she'll prescribe T3. If not, I don't see any point in continuing with endos and will self medicate. I'll not worry about bloods, other than thyroglobulin twice a year and my GP surgery can run those.
Hi Clutter, that's quite a lot you've had to go through, way over my head, and I certainly hope you have been receiving advice and support on this forum as they seem pretty clued up and empathetic. I doubt I have anything as serious as nodules, never mind anything worse, but I guess one never knows unless an ultrasound is carried out. But in any case my next step will def be requesting blood tests for : thyroid antibodies
iron , ferritin (ferritin must be at least 70 or you cannot utilise thyroxine) and folate, b12 and tests to rule out pernicous anaemia.
Nodules are common and only become troublesome when they get a bit big and press on a nerve or windpipe, gullet etc. Any form of thyroid cancer is quite rare, although it's one of the fastest growing which kinda suggests environmental influences.
Sites like this will have saved me decades of illness by making me advocate for my own care and recovery rather than waiting for the 'professionals' to cure me.
Good luck with your tests. Have patience, but not too much.
Thank you Clutter. Amazing how incompetent GP's are, even in diagnosing cancers eg my sister and friend had text book symptoms of their particular cancers, after non-diagnosis over several years of compaints of these symptoms, my sister had to have her cervix and ovaries removed, my friend died at 61 of his lung cancer.
Sorry to hear about how your family and friend were let down.
In all fairness, my GP was excellent, running & re-running tests where results didnt gel with symptoms and in referring me promptly to an excellent surgeon based on clinical symptoms and ultra sound scan. Sadly she's left the practice.
Its the endocrinologists post surgery that im not happy with, and the GPs deference to the 'specialists'.
Hi reallyfedup123, as well as the tests you recommend: thyroid antibodies; iron; ferritin and folate; b12 and tests to rule out pernicous anaemia, I think I should ask for T3 and FT3 judging by: ' T4 is the storage form of the thyroid hormones, and it must be converted to the active form, T3, before your body can use it. Some of us convert too slowly, so even though FT4 levels are good (or even a bit high in your case), FT3 levels remain low. As long as FT3 is low, you will not feel well. This can be remedied by lowering T4 meds a little and adding a direct source of T3 meds. FT3 often has to be in the upper half to upper third of the range before symptoms are relieved.'
Do you think I should also be asking for a blood calcium test? Anything else while I'm at it?
Thank you for educating me on this reallyfedup123, will report any developments.
Hi reallyfedup123, he did add FT3, so hopefully will get a result on this.