When I read members’ experiences of prompt PMR diagnoses I’m truly pleased for them but I have to admit to feeling a degree of envy. My diagnosis arrived ‘only’ five months after onset of symptoms; I say ‘only’ because I know that for others the wait was far, far longer: PMRpro, for example, was without treatment for five years! This is hard for me to even contemplate!
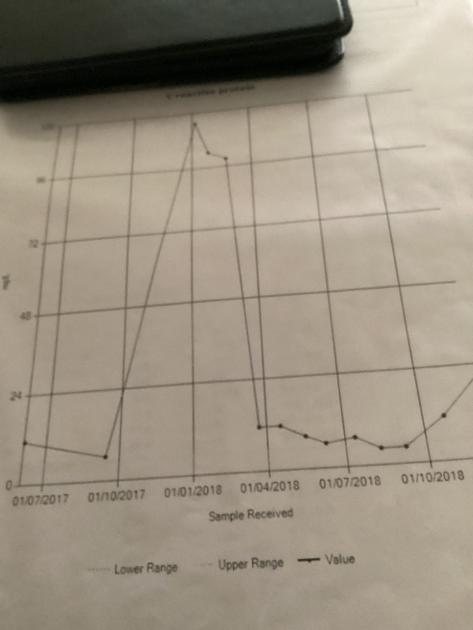
My own relatively short undiagnosed journey to the eventual prednisolone and blessed relief consisted of increasing symptoms and approximately two-weekly blood tests where after each one the GP read my results and apologised for being unable to suggest a cause of my increasing pain that was gradually affecting every part of my body from head to toe and fingers: inability to lift hand to mouth, daily weight loss, non-existent appetite, weakness from head to toe, deathly pallor and eventual CRP level of 115 -see above (ideally should be below five).
It was after being told for the eighth time, “We are still trying to find out what is wrong” that I crumpled and told the GP that I couldn’t go on for much longer. I shuffled out of the door, hunched over and in extreme pain out after having to be hauled up from the chair because there wasn’t a hope in h*!! that I could manage to independently stand from seated. Within a week I was referred to Rheumatology and thankfully found myself in the care of a renowned specialist who had spent most of his working life researching PMR and GCA/LVV.
Lately, I have come to believe there must be a link between late PMR diagnosis and lack of treatment where inflammation in the body is allowed to build up to such high levels and lead to Large Vessel Vasculitis and aortic aneurysm and/or other conditions.
My GP could see my rapid physical deterioration and worrying blood test results.
Why wasn’t inflammatory disease investigated?
Would my aneurysm have been prevented if I’d been diagnosed sooner?
I don’t think I need to ask if my GP (kind though she was) was lacking in knowledge/awareness of PMR.
I would be interested to hear from others who have had a similar experience of LVV after delayed treatment for their PMR.
Thank you for reading this 😘.