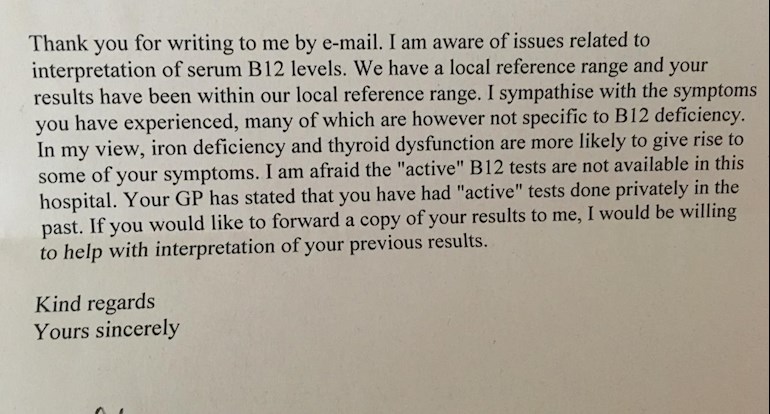
So I wrote a letter to the consultant at the nhs who is refusing to see me even thought my gp referred me to him. Please see below, I’ve attached the consultants response. Any help on where to go now?
Thanks
(B12. 215 range 180-2000)
I hope you don’t mind me emailing yourself but I am really feel let down by your decision not to treat me according to NICE and the BNF guidelines.
My gp recently wrote to you to ask if you would see me in clinic due to my long standing symptoms and blood test results.
You wrote in the last letter to my GP that there is no evidence to suggest that I have a b12 deficiency, I would like to know how you came about this decision? You also state that I have had 3 “normal” total b12 serum test results this year.
According to the nhs and I quote the below paragraph from the nhs website
(However, some people can have problems with their normal levels of these vitamins or may have low levels despite having no symptoms. This is why it's important for your symptoms to be taken into account when a diagnosis is made.
A particular drawback of testing vitamin B12 levels is that the current widely-used blood test only measures the total amount of vitamin B12 in your blood.
This means it measures forms of vitamin B12 that are "active" and can be used by your body, as well as the "inactive" forms, which can't. If a significant amount of the vitamin B12 in your blood is "inactive", a blood test may show that you have normal B12 levels, even though your body can't use much of it.)
I have numerous symptoms of b12 deficiency I shall list some below:
· Tinnitus
· Paresthesia - numbness, tingling
· Dizziness
· Restless legs
· Forgetfulness
· Anxiety
· palpitations
· IBS - Irritable bowel syndrome
· Constipation
· Glossitis
· Fainting/light headedness
· Repeated ear infection
· Headaches
· lack of energy
According to the BNF guidelines
1. The clinical picture is the most important factor in assessing the significance of test results assessing cobalamin status because there is no ‘gold standard’ test to define deficiency.
2. Definitive cut-off points to define clinical and subclinical deficiency states are not possible, given the variety of methodologies used and technical issues, and local reference ranges should be established.
3. In the presence of discordance between the test result and strong clinical features of deficiency, treatment should not be delayed to avoid neurological impairment.
I am concerned that I am not being treated correctly for my neurological symptoms. I know that to have the best chance of completely reversing these I need to be treated as per NICE and BNF Guidelines 9.1.2. which state that injections should be given every other day until symptoms stop improving. Please note; there is no time limit on this and I understand that in order to reverse neurological symptoms it could take some time.
Thank you for taking the time to read my letter
Kind regards