Can anyone help tell my daughter what to do next? She has been coping with a busy job and family with terrible symptoms of fatigue and weakness. A couple of years ago I persuaded her to go to the doctor but she was just told she was bound to be tired with her lifestyle and more or less fobbed off. After fainting recently, she went back to the GP and she was finally given blood tests and these are the results. She was told to take B12 and iron supplements but not given any more advice . She is 46 years old and has been a vegetarian since she was 14. Can anyone help me? I want to advise her but have very little knowledge of her problem. I can only seem to get one part of the blood test results she has sent me in this post - I will do a 'Part Two' for the rest!
Finally had blood test: Can anyone help... - Pernicious Anaemi...
Finally had blood test
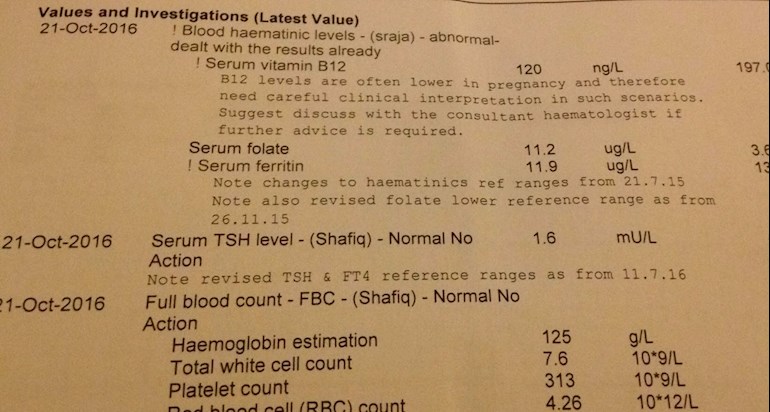
P.S. I see I cropped out the ranges when I removed the personal info.....
Range for B 12 is 197 - 771, range for serum folate is 3.60 - 18.7 and range for ferritin is 13.00 to 150.00
Ferritin is a protein that binds to iron so the body can use it - being low is an indicator of an iron based anaemia though her haemoglobin doesn't actually look low but that may be because the iron based anaemia is pushing the bloodwork in the opposite direction from a B12 deficiency - which tends to make red blood cells larger and rounder - increasing the haemoglobin content.
Sounds like your daughter's GP is assuming that your daughters B12 deficiency is due to diet. Unless she is avoiding dairy, eggs and doesn't eat breakfast cereal that is actually highly unlikely - and much more likely that she has an absorption problem.
If she has an absorption problem then the tablets that she has been given aren't going to be sufficient to ensure she is getting enough B12 - as the tablets she has been given are presumably 50mcg.
Suggest you
a) review your daughters diet and work out how much B12 she is normally consuming - you'll have to google for B12 contents of foods she is taking in - or look at the packets if it is fortified cereals. If she has been supplementing B12 in any way shape or form from a daily vitamin supplement then make a note of that. - aim is to demonstrate to GP that your daughter has been taking in the daily RDA for B12 which is about 2.4mcg to refute any tendency to assume that the problem is dietary.
if it turns out that your daughter hasn't been getting enough B12 in her diet then try the tablets for a while and see if things start to improve - if not then go back to the doctor again
b) Put together a full list of your daughters symptoms
pernicious-anaemia-society....
c) look through the pinned posts for materials on diagnosis and treatment of absorption problems - as there are a number, though guidance tends to focus on PA which is the most common and not make GPs aware that there are actually other problems.
You could ask for an IFA test to be done to rule out PA - but be aware that this is prone to give false negatives about 50% of time so won't rule out PA
d) go with your daughter to see the GP and get them to recognise that the problem isn't dietary and your daughter needs to be put on loading doses, followed by maintenance doses.
Also, if your daughter has ever had any gastric surgery that may have affected the ileum then you should make sure her GP is aware of that
Thank you so much for your detailed reply, Gambit. I am very grateful. My daughter tells me her doctor has booked her in for another test to check her 'absorption' so presumably she is now thinking pernicious anaemia. Is that right? If you can't absorb enough B12 through diet, that means PA? What does the absorption test involve? Unfortunately, I can't go with her as I live in Spain and she is in the UK. Thanks again for getting back to me so quickly. I am actually furious with her GP as my poor daughter has been struggling for such a long time.
Sorry, just re-read and you do say absorption problems can be due to causes other than PA - will look at the link you suggest. She did have an op 4 years to remove a dermoid cyst on her ovary (ovary also removed). Would that have had an effect, do you think?
yes, sounds like GP is doing the IFA test - but note the caveat on the accuracy of that test - and GP probably isn't aware of that.
There are lots of things that can cause a B12 absorption problem - PA is just one of them - though it is probably the most common
99% of B12 is absorbed in the ileum - excess is stored in the liver and then released into the ileum in bile for reabsorption - so if there is an absorption problem it can take a long time for it to become a fully blown deficiency - but once it starts to bite symptoms tend to balloon.
PA is an autoimmune problem that basically attacks the absorption mechanisms in the ileum
surgery affecting the ileum will cause problems
h pylori infection can cause absorption problems
lowering levels of stomach acidity affects absorption - as the symptoms are basically the same as high stomach acidity it is often treated with things aimed at lowering stomach acidity making the problem worse - PPIs are a particular problem area
drug interactions can also affect B12 absorption - including PPIs, NSAIDs and metformin used to treat type 2 diabetes.
which is a long way of saying that there are more absorption problems than PA - and treatment is the same whatever the absorption problem ... though dealing with a h pylori infection is in theory curable.
Unfortunately too many of us struggle with health problems in UK. GPs unwilling to help. Too well paid for not doing a great job! They have a serious ingrained attitude problem.... although there might be a handful of rare good GPs. I only wish I could find one right now as am seriously struggling too. Better luck for your daughter. Do hope someone will finally help her.
Dreadfully low ferritin too,
She must be feeling terrible. Take ferrous fumerate or bisglycinate to raise iron storage levels. Aim for serum ferritin of 80 .. the level at which hair loss stops, and fatigue reduces. She is in danger of feeling v anxious, panic attacks, hair loss and restless legs syndrome at this low iron storage level. Lucky her, to have you fighting for her.
Thank you, Aspmama. When her GP sent her away with instructions to 'take supplements' but no recommendations, I did a bit of research and suggested she get Solgar Gentle Iron 25mg, which I see is bisgylycinate, so hopefully that is going to help, also Solgar sublingual methylcobalamin 1,000 but maybe she should get the 5,000........although if she does have an absorption problem (still to be discovered) that won't help, I suppose. I appreciate you replying, thank you.
Hi,
Causes of B12 deficiency
b12deficiency.info/what-are...
b12deficiency.info/what-to-...
B12 books
"Could It Be b12" by Sally pacholok and JJ. Stuart
"What You Need to Know About Pernicious Anaemia and Vitamin B12 Deficiency" by Martyn Hooper
UK B12 websites
b12deficiency.info/ Lots of useful B12 info and interesting B12 blog.
pernicious-anaemia-society....
martynhooper.com/ blog by chair of PAS
If you are UK based, I'd recommend reading the following
1)BCSH Cobalamin and Folate Guidelines. Three quarters through document is a flowchart that shows the process UK doctors should follow with someone who has low B12 and/or is symptomatic for B12 deficiency. A quarter through document is info on UK b12 treatment doses etc.
b-s-h.org.uk/guidelines/ Click on "Diagnosis of B12 and Folate deficiency"
2) BMJ B12 article
Link about writing to GP if unhappy with treatment. Does not seem to mention BCSH Cobalamin guidelines which i do if I write about B12.
b12deficiency.info/b12-writ...
B12 deficiency in families
pernicious-anaemia-society....
It may be worth mentioning to GP if any blood relatives have PA or another cause of b12 deficiency or other auto-immune conditions. PA can run in families. Has your daughter ever had a test for Coeliac disease? Thyroid disease?
coeliac.org.uk/coeliac-dise...
IFA test
"has booked her in for another test to check her 'absorption' so presumably she is now thinking pernicious anaemia."
This may be the IFA test (Intrinsic Factor Antibody). be aware that this test is not always reliable...it's possible to still have PA even if IFa test is negative. The flowchart I mentioned in the BCSH Cobalamin and Folate Guidelines mentions when someone can be diagnosed with Antibody Negative PA (PA where IFA test is negative).
I'd also recommend reading the summary fbirder compiled. Link on his profile page or in third pinned post (last link in list). lots of useful quotes from mainly UK b12 documents. I found this useful when faced with doctors who hadn't done their homework on B12.
Nitrous Oxide
If your daughter has had surgery in the past, was nitrous oxide used?
gov.uk/drug-safety-update/n...
I am not a medic just a person who has spent years trying to find answers.
I gave my GPs a copy of Martyn hooper's book, a copy of the BCSH Cobalamin guidelines and the PAS symptoms checklist with all my symptoms ticked plus added others that weren't on list.
Gosh, that should keep me quiet for a while lol. Thanks for going to all that trouble, Sleepybunny, I will read your links. Daughter had a TSH test with all the other blood tests, I think that result was in my Part Two post, as my daughter sent me her results in 2 photos, so I put the other results in another post. I think her TSH was 1.6......it looked OK, anyway. No, she's never been tested for coeliac disease, maybe that will become necessary.
Thanks again, such kind people on this forum!
 Thank you so much, that is going to help us such a lot. You are a star, Gambit!
Thank you so much, that is going to help us such a lot. You are a star, Gambit!