This is a long and not cheerful post, I understand if you don’t wish to wade fully or at all thru it. Sections are marked for easy reference. The thoughts are my opinions only.
--
I wrote a few months ago on my botched flu vax anniversary. Today is the one year mark for my Last Dose of Besremi, step 2 into the abyss. Some thoughts, regrets, and I hope some lessons.
A summary: I was on Bes for 11 months. Great therapy. A flu vax went bad ~month 9. Continuing on Bes I got some new warnings. I opted to take a last dose, and immediately it blew up. One simple life changing choice. I now have aggressive onset Sjogren’s.
Details preceding Last Dose (this is mostly in prior posts
I switched from HU to Bes Feb ’22. I felt ok at the start, up to ~70mcg and held CHR. But Dr wanted to hit 200 in hopes to get best VAF reductions. We topped out at 140 for low WBC.
The post here had some real time thoughts on my dosing. My Dr scolded me for not asking permission to reduce it before this trip (this is relevant later). Throughout my Bes journey past 100mcg I had malaise etc. We resumed afterward at 140 till ~the end but I always felt ~50-70 was where I would feel better.
healthunlocked.com/mpnvoice...
In Nov ’22 I rushed to get the Covid and Flu vaxes after another trip as they predicted a bad season. I opted for the Moderna covid as it is a larger dose than Pfizer, and more seemed better. One week later I got a flu vax, Flublok brand at the same pharmacy, also higher potency. (I have old posts on this)
Immediately after the flu vax I sensed wrong. A whole body weirdness and never before but brief pain in right knee joint. I wish it had been just an allergic reaction. Over next days shoulder pain at the vax site which grew to 8/10. A neurologist Dx Brachial neuritis, a known rare vax risk. Most neuro vax events improve over months or years, but can precede other things.
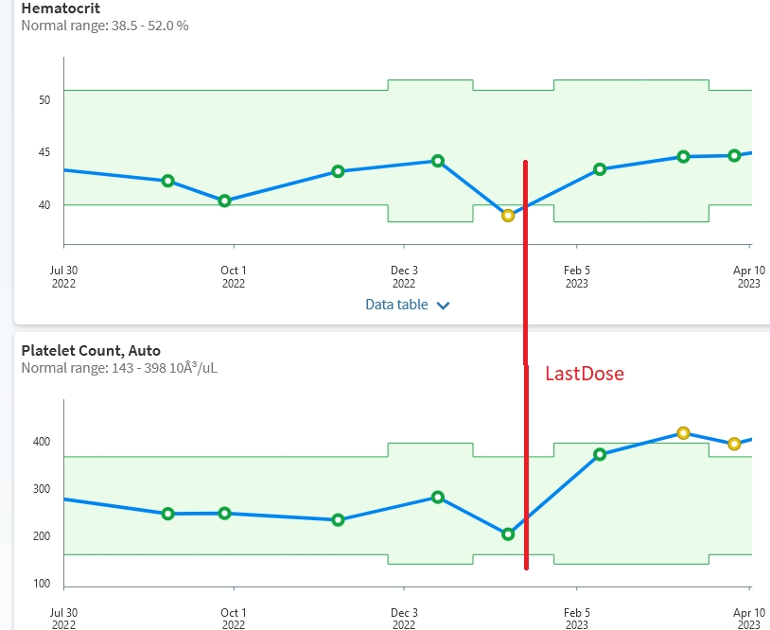
By new year ’23 neuro was less severe. But on Sunday Jan 15 I was at parents’ new retirement home helping assemble furniture. During dinner I felt a sudden fatigue and malaise of a new sort and had trouble with the further work. Bad vibes continued the next days. The plot here shows my HCT, PLT were reacting too well just prior to the Last Dose. My next Bes dose was due Wed.
My Last Dose, Wed Jan 18
I sent Dr my concerns and asked about reducing or pausing the IFN. This is advised in the FDA label but the urgency part is not clear. Dr got back to me Thurs. Meantime (see “scolding” note above) I didn’t want to change the schedule without confirmation. In fact it was an emergency but I had no clue (do “bad vibes” meet the criteria?). I took a reduced dose of 100mcg late Wed. Within minutes I couldn’t sit up so I went to bed. I stood up ~ an hour later and totally passed out. I hit my eye socket on a low table and twisted my neck which I knew only days later from the bruise.
Aftermath of Last Dose
A few days after the pass out I got eye flashes, eye Dr checked retina, ok so far. For the next couple months I deteriorated. ER visit was not useful. Short episodes of paralysis, twitching on the floor, passing out after eating, leg collapse, general neuro trouble. I needed a walker occasionally. Several episodes felt like a stroke and imminent demise. Thru the summer it developed into obvious Sjogren’s including unprompted disabling anxiety. I had two periods of feeling ok but now all social activities are out. I’m currently in a fairly stable level of misery.
Why worry about Sjogren’s?
A simple internet search will bring up a mild autoimmune disorder that just causes nuisance dryness.
- In fact it is for many victims an (emotional) Death Sentence - . One Voice member with reason to know agrees with that description. I asked my Rheum Dr which rheum disease is the worst with regard to treatments vs symptoms, his answer “Sjogren’s”. You don’t want to catch it. It’s too often a whole body wrecker. I won’t go in to the details. This site has a good reality for understanding the affliction:
--
Here is a sample from our own HealthUnlocked. this is our reality of this whole body disease and maybe my destiny:
healthunlocked.com/lupusuk/...
"I experienced a dramatic deterioration with teeth and gums 2 years ago, dentist advised I would lose all my teeth within 6 months and because of the lack of saliva..."
"Sjogrens as you know is a nasty illness which is now brutaly attacking my joints, the pain is excuciating !"...
"Your rheumy is very ignorant of how much damage sjogrens can do and i'm afraid needs to be educated. I would be batting him some information."
--
Why should MPN pts worry about Sjogren’s?
No special attention is required except when on IFN therapy. A botched vax is not required. A surprising number of members have been affected to some extent. Sjo is the Auto-Immune (A-I) for which IFN is most specific (other than thyroid issues). I know of no studies checking why this is so, but Medicine's poor grasp of Sjo is one likely reason for its low visibility.
In the Euro label Sjo is the only (non-thyroid) A-I listed as “common” (1-10% pts) on page 9 here:
ema.europa.eu/en/documents/...
At least Sjo is at the lower end of common. I’ve seen it up to ~4%, but can’t find that reference right now. But in any case a disease this dire rated as “common” needs our attention. Also listed as common is antinuclear antibody (ANA) positive. This is a broad warning of potential A-I events and should be part of monitoring, see “what to do about it" below.
The US FDA in fact gives A-I worthy attention, this is the Black Box warning that I didn’t give a thought to while on Bes:
“Interferon alfa products may cause or aggravate fatal or life-threatening neuropsychiatric, autoimmune, ischemic, and infectious disorders. Monitor closely and withdraw therapy with persistently severe or worsening signs or symptoms of the above disorders”. The unsolved question is what actual events meet the “withdraw" guidance?
Of all these FDA severe outcomes, only A-I in the form of Sjo is “common” per Euro. So in effect FDA black box is warning us of a "common" outcome. Importantly Sjo is rarely fatal, designed best for lifetime suffering.
--
There are other Voice members on IFN affected by Sjo, in my rough guess from the forum at about the range above 1-4%. Some of the Voice members affected with Sjo quit IFN in time. There are more than one for whom it is likely too late. Sjo is prone to a point of no return.
The pegylated IFNs (PEG/BES) have improved tolerability, but there is a flip side to this I now appreciate. The advantage of long duration becomes a hazard when there is an urgent need to get the IFN out of the system. It’s likely one reason my Last Dose did such damage over the next month. Support for acting quickly when warranted.
--
The report below discusses IFN being a contributor to Sjo:
“In (Sjogren's) disease, a large number of studies have shown that an overexpression of type I IFN (the type we use)… is present …this finding is associated with the development of systemic extra-glandular manifestations (this is the extra nasties in Sjo) … inhibition or modulation of IFN signaling has been regarded as a potential target for the therapeutic approach”
ncbi.nlm.nih.gov/pmc/articl...
Hence some emerging therapies seek to reduce active IFN. When Sjo is brewing adding more IFN should be contra indicated as it clearly was for me. (There was a time ~1999 where IFN was explored as a therapy for Sjo, but this idea is not current) Clearly this is a problem only when Sjo is present or imminent and most MPN pts are not at risk.
What to do about it? (My opinion)
IFN is an amazing therapy. But it is twitchy. My Dr called it tough medicine and preferred I select Rux. IFN seems unique in our meds in its widely varying effective doses and surprise and suddenness of some its effects. FDA says “withdraw therapy with persistently severe or worsening signs…” My blood count plot here shows something was brewing, the IFN was suddenly working too well just prior to the Last Dose. A sudden increase in general fatigue/malaise without a dose change was my main but too vague indicator.
I suggest if you get new dryness in mouth, eyes, or women’s private parts, and meds haven’t changed, this is time to stop IFN asap and then discuss with your trusted expert. But dryness is optional and if present often starts after the disease is well underway. My case is an example of pre-Sjo hiding as other things. Neuro for example preceded overt Sjo so a dryness indicator would not have helped. Another stop sign is upon an adverse vax reaction (esp neuro issues, not the typical aches and fevers) stop therapy asap and then discuss with your trusted expert. One member saw my posts on this vax angle too late.
--
This old post may have a relevant item. I had plenty of fatigue/malaise on IFN, maybe it suggests extra care required:
“Patients who develop persistent fatigue experience greater increases in IL-6 and 10 in response to IFN-α …(IFN-a, the old non-peg) induces a persistent fatigue in some individuals, which does not abate post-treatment”
healthunlocked.com/mpnvoice...
I recommend IFN pts get regularly monitored for at least the basic set of A-I (autoimmune) indicators. including rheumatoid factor, (RH) c-reactive protein (CRP), erythrocyte sedimentation rate,( ESR), and (ANA). ANA positive is “common" in the Euro label. A full list of all tests I got is in another post today. But these can sometimes all be negative even with severe Sjo, I had only a single positive among all these.
I wish I or anyone could advise more solid ways to know how to predict IFN black box AEs. I also wish someone had posted this before Nov 2022, I would have stayed safe.
IFN Dosing
My opinion: The idea PharmaEssentia is promoting of aggressive dosing (ie starting at arbitrary 250) vs dosing for response is malpractice. The added risk is not rational even if it might (unproven) get a few more VAF points. If it’s that urgent to cut HCT asap get a phleb or take temporary HU if tolerant. I made a plot a while ago of members’ early dose and CHR response, link below. Not a scientific study at all but it showed most those with good CHR response got there on doses way under 250. Low and slow is a theme we’re seeing here, my experience supports and helps inspire this policy.
healthunlocked.com/mpnvoice...
I tried repeating this survey more recently but the response was too sparse to make a plot.
Is there any hope if one has Sjo?
The bad place is moderate to severe disease. I have moderate and aggressive onset. But it can be and stay mild for a long time. Re IFN - timely withdrawal makes mild more likely. For women (9/10 cases) on avg it is less severe. There are finally effective agents post phase 2 or starting phase 3. One problem in trials has been how to even measure the disease, it affects something and/or everything. One theory I've seen on A-I is being a software bug in liver signaling. So acting there might be the cure way in the future
Any other serious IFN effects among members?
I’m aware of a couple: One had deafness, reversed after stop of therapy (“uncommon” in Euro label.) Another had kidney failure ("uncommon to rare”), shortly after starting and then quitting Bes, preceded by mild A-I issues, slowly recovered.
Vaccine strategy
More may not be better. The Moderna shot is 50mcg, Pfizer is 30. Some early evidence showed the Mod was more effective, I’ve posted on that. But for those on IFN, Pfz may be the more conservative choice. On timing, please never get any shot one week after a prior one unless it’s actual protocol. I believe this is one source of my wreck. Two weeks minimum is safer. For me I won’t get an in-arm flu shot again, I’m high risk, it is not that effective (~50% best case when well matched) and the risk is every year. For Covid and maybe flu, I plan to await the next gen nasal vaxes, these should be lower risk and more effective. For those without a history of adverse reactions, these worries are minimal but the 1week contra indication stands in my opinion.
My benefits on Bes
I did have some of the best benefits of IFN. Blood counts were perfect, even CMPs were flawless, so the black box wasn’t predicted by CMPs in my case. VAF declined well, but seemed to be heading to a lowest limit. Widely spaced dosing was very convenient. My eyesight focus improved and this has persisted.
How about Rux and HU?
These do not share the FDA black box. I’m not aware of severe irreversible adverse events caused by these meds, doesn't mean it hasn’t happened. Rux does have a high risk if quitting cold turkey. Any members with more info to help guide us on signs and prevention of severe outcomes for these is most welcome.
This is an old thread on AEs for Rux and IFN. My take, while I was on Bes, was Rux had fewer high risk events.
healthunlocked.com/mpnvoice...
Conclusion
I’ve put two days into this heartfelt post. I hope it can help protect even just one more member. Researchers should look deeper into the IFN A-I markers and give us something to monitor. Best conclusion I can offer is “Low and slow” and be ready to act on any A-I like emergent.