I've posted on other threads about INF treatments. I decided to start a new post since I just came across a most relevant study that should wake up our doctors if they are paying attention. In any other cancer I think this result would be called revolutionary, but since ours is such a slow motion and rare journey, the medical field doesn’t get worked up.
It compares INF (Interferon) , HU (Hydrea) and Phlebotomy for Jak2 PV over a very long time, starting in 1966 to 2019. The triple comparison is neat by itself. It was most recently published this year. In my opinion it should be relevant to the other MPNs since the current standard PEG seems to be effective in many of the things we all care about. But it is specific to “well defined” PV.
The authors are from an institution that was among the earliest to start trying INF.
This study follows the old fashioned rIFNα, not the peg versions, since PEG was not available back then. We can hope that PEG and Ropeg will have at least this or better results since the basic actions are similar but they are easier on the body.
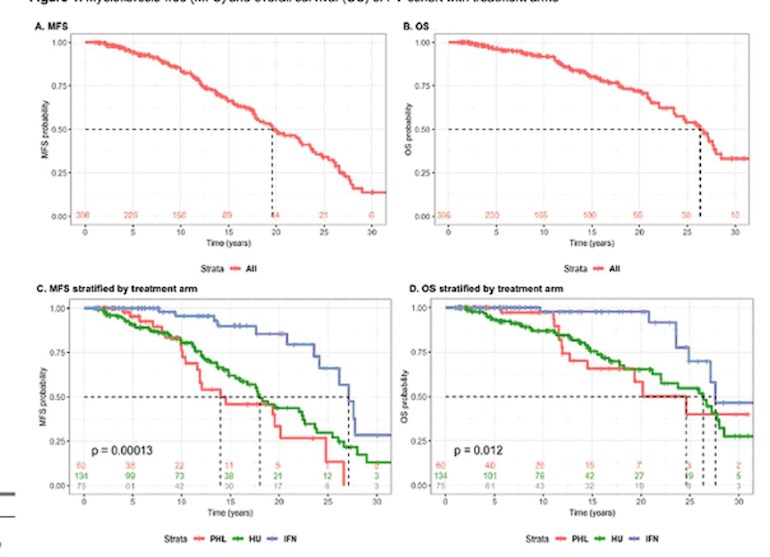
Below is a summary from the report. MFS is myelofibrosis-free survival, OS is overall survival.
-----
-Low Risk- (generally under 60)
--20 year MFS /OS--
INF: 84% / 100%
HU: 65% / 85%
PB: 55% / 80%
-Hi Risk- (Generally over 60)
--20 year MFS /OS--
INF: 89% / 66%
HU: 41% / 40%
PB: 36% / 14%
====
My take is INF is the best way to stay MF free and live singif longer.
This adds to the trend supporting 1st use of INF with hope that Ropeg
will open up the option more more of us. Low risk generally means under
60 years, high risk over 60 or with other risk factors.(prior clots
etc)
At the top is one of several graphs in the report. In the lower set the green and red lines are Phleb and HU. The blue one is INF. Note how much higher the blue lines stay for so many years. The authors are not impressed with long term HU.
If you’re up for it, read the reports, links below, and let us know your thoughts.
onclive.com/view/interferon...
ashpublications.org/blood/a...
Audio from Author: