Hi All,
My Father was diagnosed as stage 4 PCa with widespread bone mets in Nov 2021. Since then he has been on ADT + Enza + Denosumab regimen (details on my profile)
His PSA had increased slightly in the last few readings but he has largely been asymptomatic
12/22 - 0.81
03/23 - 0.83
06/23 - 1.21
Based on the above our Oncologist suggested a PSMA scan and a repeat of PSA test which we did yesterday . The latest PSA score was 1.18 (07/23)
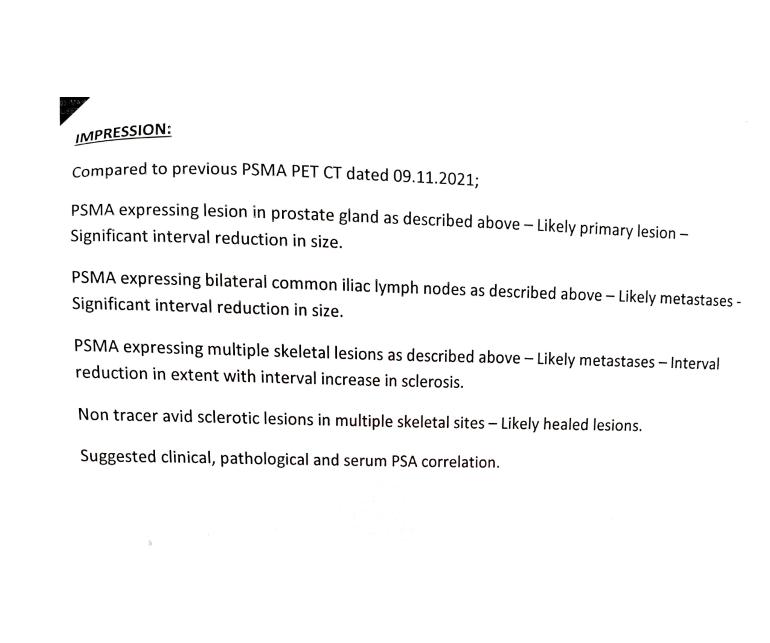
The scan did not find any new mets and found significant reduction in the old lesions, I have attached the results of the Scan below.
While we are happy to see the latest reports there are few queries I hope someone can answer
1. There is apparently an increase in PSA as seen with the repeat test but the PSMA scan has only detected reduced mets and no new mets. Only the prostate and a lymph node close to it show active uptake , if so what is behind the rise in PSA ?
2. As per our Medical Oncologist this could be due to either micro metastatic activity increase or because of the active lesions becoming resistant. For the former we have to wait and watch, If we assume the latter then he has offered us SBRT radiation to the prostate and lymph node lesion after consulting with RO, he believes this will improve overall survival. The problem here is that they are not definite about it and suggestion was based on "if then .. it may" scenario
Given this can folks here recommend how to go about it :-
a. Wait and watch with more frequent PSA readings
b. Go for the SBRT suggestion
c. Any other suggestions here ?