Okay guys, I'm asking for your insights....
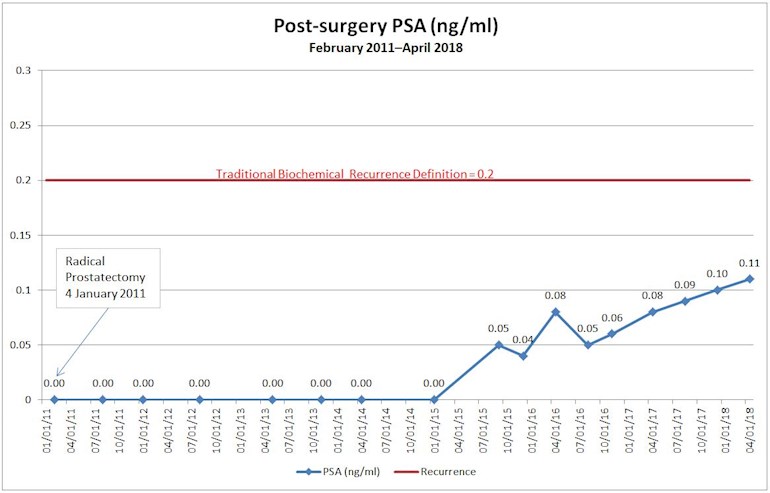
I was diagnosed in November 2010 and had a radical prostatectomy in January 2011 (3+4, pT2c N0 M0, negative margins, no extra capsular extension, no seminal vesicle involvement). My post-surgery PSA remained undetectable for 54 months and then came in at 0.05 ng/ml in September 2015. Last month it came in at 0.11 ng/ml.
Next week, I have my first appointment with a radiation oncologist to open the discussion and learn about salvage radiation therapy.
I'm compiling my list of questions for the radiation oncologist and I'm wondering, for those of you who have been on a similar path, what are the one or two questions that you thought, "Oh, crap! I should have asked that," but didn't in your first visit discussing salvage radiation therapy.
Thanks in advance!
—Dan