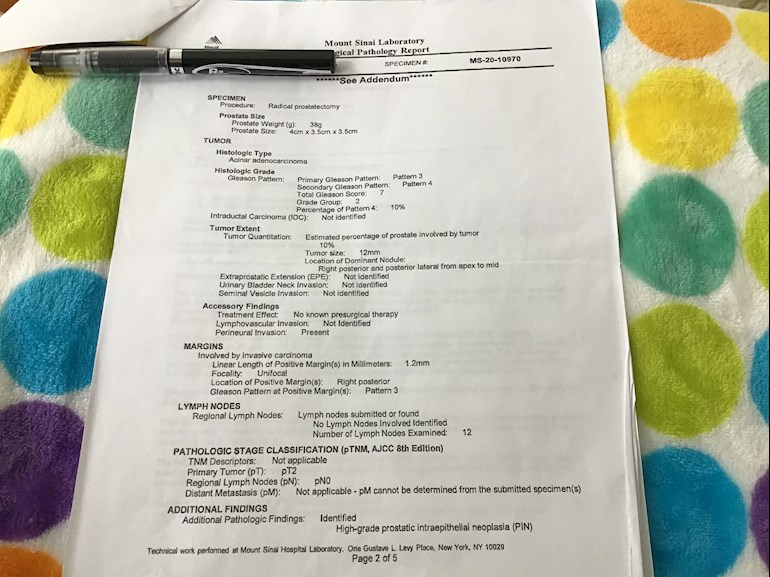
Hello, I am new to the site! Age 65. Was diagnosed in January 2020 with prostate cancer. T2a Gleason 7 (3+4) PSA 5.71 Robotic Prostatectomy done 6/13/2020 by Dr. Ash Tewari at Mount Sinai. One year of undetectable PSA, then rose to 0.1 in 11/2021. I had a flare up of diverticulitis in 12/2021! My GP ordered a CT Scan with contrast that showed a swollen iliac lymph node in the pelvic region, so ordered PSA that came back 0.2. I am seeing a Radiation Oncologist tomorrow in my area, Dr. David Hauerstock. Can anyone tell me what questions I should ask and what treatment is the first line of defense? I am including a photo of the Pathology Report . Any advice would be greatly appreciated! and thanks to all the people and information on this site.
Questions to ask the Oncologist for u... - Advanced Prostate...
Questions to ask the Oncologist for upcoming visit tomorrow!
What makes you think that this swollen iliac lymph node is due to prostate cancer ? I think its more likely due ti diverticulitis (inflammation of colorectal area) PSA 0.1 or 0.2 is insignificant finding unless PSA keeps rising continuously for next 3 to 4 times.
Thank You for the info! Could diverticulitis cause PSA to be elevated? This is what I was hoping!
I would try to get a PSMA scan to evaluate. I think the scan would be helpful in determining cancerous lymph nodes versus reactive nodes.
Go to PYLARIFY website and see what’s closest for you. This was recently FDA approved and more centers are offering. Has much better sensitivity in diagnosing metastasis than bone scans or CT. You need to know where the PSA is coming from.
Hello Tall_Allen, Thanks for the great info, As far as side effects! everything has been great, No pads! No problem with erectile dysfunction! Everything has return to almost 100% pre RP. I am experiencing some of the same discomfort in the pelvis buttock region as when first diagnosed. That's the kicker, everything has been going so fine! can you tell me what are the important questions I should be asking the Radiation Oncologist? PS I do not live in the NYC region! I'm in upstate NY. Thank You Much
That is one of the clearest laid out pathology reports I have ever seen. And Ash Tewari is certainly a master. How are your side effects - incontinence? erectile dysfunction? If they are still troublesome, you may wish to start ADT now to give yourself more time for healing before radiation begins.
What the RO will probably recommend is salvage radiation to the prostate bed and the entire pelvic lymph node area. The dimensions of the radiation area has recently been expanded. I'm sure your RO is aware of it, and you may wish to bring it up. There may be anatomical reasons why the expansion may or may not be good for you in particular:
prostatecancer.news/2021/05...
The RO will also give you an extra boost of radiation to the enlarged lymph node. To be sure, it is a good idea to get a PSMA PET scan to find any other lymph nodes that may be too small to show up on a CT scan. Mount Sinai ( as well as several other hospitals in Manhattan) now offers the "Pylarify" PSMA PET scan. It is covered by Medicare.
There is a clinical trial now at Memorial Sloan Kettering (Craig Grossman) to test this strategy for men with exactly your situation. You may wish to get in on it. Here are the details:
clinicaltrials.gov/ct2/show...
There is every hope it will be curative.
With the Pylarify scan, does being on ADT reduce it's sensitivity? In other words, scan first then ADT or ADT then scan is ok?
Detection is very PSA dependent, it would be detected only in a minority of cases where PSA≤0.2.
For about a month, maybe two, ADT may actually increase expression of PSMA on the cancer surface, making the cancer more detectable. After that, it reduces expression of PSMA, making the cancer less detectable.
Thanks, When I typed the rising PSA it is actually 0.2.4
metastases with rapidly rising PSA often show up, even when the PSA is low. Here's the Pylarify site locator:
Good Morning Tall_Allen, Had the visit with my RO on Wednesday! He reviewed the CT Scan that showed the swollen iliac lymph node and said it wasn’t cancer and could be resulted from the surgery? I hope he’s right! Also will call today for the latest PSA results? If treatment is needed? He will contact Dr. Tewari’s office for there recommendations going forward with treatment. Is there any reason why I shouldn’t have treatment done locally? or should I go back to Mount Sinai or some other cancer center? The problem is NYC is 6 hours from my location. The RO Dr. Hauerstock seems very good, answered all my questions and is open to my thoughts! Thank You for the Pylarify site for locations near me! Hope the scan is covered by Medicare? No sure if or when I will be needing it? Thanks
It's easy enough to see if the enlarged LN has cancer. You are recurrent after RP, so you qualify for Pylarify now. It is covered by Medicare. If you do that first and can rule out cancer in pelvic LNs, you can get your SRT anywhere. If it isn't benign, I encourage you to think about that clinical trial.
Thanks for your reply! RO was talking about 3 months ADT and then 6 weeks of SRT if my PSA rises. Should here back on the PSA today. Also if ADT is the first part of my treatment? Should PSMA Scan be done first? Can I ask why, would this clinical trial be important for me? Thanks
PSMA expression increases during the 1st month of ADT, but decreases thereafter.
The clinical trial may provide hormone therapy enhancement that you otherwise would not be able to get. Even if you are not randomized to get the intensified hormone therapy, the ADT+SRT you would receive are usually top notch on a clinical trial. But it is only if the LN is positive.
Good Morning Tall_Allen from HarGreg, I spoke with my RO on Wednesday! As I stated before my PSA was undetectable for 16 months! Then on 11/13 came back at 0.1 then 0.24 and the results on Wednesday was 0.26 My question is, how do I know if and when treatment is needed? and will a PSMA scan detect anything with this PSA or do they treat blindly? Still waiting for Dr. Tewari’s input! I’m sure it will be this coming week. Thanks
You have a very personal format for decimal numbers. Is 0.2.4 or 0.2.6 0.24 and 0.26?
I don't know what 0.2.4 means. I don't know what 0.2.6 means.Look at the report again and tell me what it actually says.
Hello Tall_Allen, I wasn’t sure how to interpret my PSA readings! I called the lab and got the last two results of 0.24 and 0.26. HarGreg
That means it's very stable, and with your low Gleason score and long time to biochemical failure, you can probably just monitor it closely for a while, if you want to.
Thanks for the info! So you wouldn’t consider this very aggressive as another person committed? HarGreg
Good Morning Tall_Allen, Just heard back from my RO! He did not get any response from Dr. Tewari office at Mt Sinai re treatment! He has been in contact with my urologist here and his colleagues at UVM and they all agree that I would do the standard 6 month hormone treatment and radiation. He said with my low PSA numbers there is a good chance cancer is refined in the Prostate Bed and a good chance of a cure. What are your thoughts? Thank You HarGreg
What I wrote above was: "That means it's very stable, and with your low Gleason score and long time to biochemical failure, you can probably just monitor it closely for a while, if you want to." This is based on what is discussed under "no/delayed treatment" in this article:
prostatecancer.news/2021/10...
This is based on the enlarged lymph node not being metastatic.
There is no need for hormone therapy at your low PSA.
Thank You, I will certainly show the no/delayed treatment article to my RO and Urologist. If I decide to monitor? How often would the do PSA testing? Thank You again for the great info. HarGreg
If a PSA next month continues to show stability, you can just monitor every 3 months
🙏🏻 Thanks for all the great information in a timely manner. Are you a PC survivor? Harlow
Yes. Some info in profile.
Good Morning Tall_Allen, Hope this note finds you well! Just wanting to pick your brain? I have an appointment with my Urologist on Tuesday 2/8 to discuss treatment/observation? If you look at my earlier post PSA went from undetectable for 16 months post RP then from 11/2021 - 01/2022 PSA 0.1, 0.24, 0.26! I am experiencing some pain in my lower back and pelvic area, could be my osteoarthritis? My question is, should I insist on a Pylarify PSMA Scan or with my low PSA, would it reveal anything? Dr. Lieb has been my urologist from the beginning and seems to be a straight shooter! Would it be beneficial for me to get a second opinion going forward? Also my RO told me that if I decide on treatment? there is a 80-90% of a cure! Could this be true? Thanks, HarGreg
Your PSA is low and stable and probably won't reveal much on Pylarify PET scan -- maybe a 1 in 3 chance. Your odds of no progression are about the same whether or not you have salvage radiation.
Good Morning Tall_Allen, I saw my Urologist yesterday and we came to the same conclusion as you stated! We will monitor for 3 months, if psa rises? PSMA scan and discuss treatment. I like the fact he doesn’t push treatment until needed! Thank You so much for the good info. Harlow
Hello Allen, Had Bone Scan, Testosterone, PSA ultra sensitive, Urine Culture analysis and Full blood panel on 04/19/22. Scan was clean, Everything else was normal, PSA was 0.24, unchanged from prior 0.26, Testosterone 475. Dr. Lieb will test psa again in one month, if psa is increasing, he will order PSMA Scan. We will continue to monitor and I hope it will be stable. . I like the fact he is not pushing radiation until need! Could a person be cured if after 2 years RP and have very low PSA that is stable? Thank You again for all your dedication and advice. Harlow
I'm not sure that "cure" is the right word, but "durable remission" is possible. Some recurrences never progress within a lifetime.
Good Morning TA, I am now monitoring my situation. My monthly PSA Lab is due next week! Is it important to use the same Lab? Also, with my PC post history, should I still be seeing my Urologist or should I have my RO involved? I do have all test results sent to him. Should I request a PSMA Pylarify scan at some point with a PSA of .24 Would it more reliable than the bone scan I had recently, that came back clean with results. I guess I am always a little anxious 😬, join the crowd, right! Thank You for expertise! Stay well! Harlow
Yes, use the same lab if you can.
As I said, Pylarify is pretty useless at your PSA.
The reason I asked is because I am experiencing discomfort in the pelvic region, dull joint pain where the bone is close to each side of rectum area, also leg area, this is why Dr. Lieb ordered the bone scan. I was DX a few years ago with osteoarthritis! Maybe the cause of the discomfort? Are there any other test that might show these symptoms? Thank You TA, Harlow
I believe that arthritis shows up on an X-ray. Ask your orthopedist.
Hello TA, As you can see by our past conversations, I am now monitoring any progression! Last Ultra PSA was 0.23, Spoke with Dr. Lieb yesterday and he is ordering the Pylarify PSMA Scan. I read your post on the SPPORT Trial Results and also on the Prostate Cancer News, maybe this is why Dr. Lieb is ordering the Scan. My question is with the new trial results, do you think monitoring is still a smart option? I also spoke to Dr. Hauerstock RO last week, he seemed positive with my low stable PSA! Thank You, Harlow
Low stable PSA is comforting, for now. I've tried to give a feeling for the "debate'" On the one hand, Alan Pollack argues for early definitive treatment (with its side effects), while cure is still possible, and it avoids lifelong ADT. Dan Spratt, OTOH, argues against treatment now because you will probably not die of PCa and you will be able to extend your life later with lifelong ADT. You have to decide for yourself between their positions.
Thank You TA for answering my questions. Would you say it is safe to monitor with PSA and scans? Could low stable psa be RP residual and not cancerous? Harlow
It is definitely cancer. PSA from any residual healthy tissue vanishes quickly. I'm not sure what you mean by "safe," but see my comments above.
I guess I am searching for the best direction at this fork in the road! Thank You
HG and TA, I had a prostatectomy about 3 years ago and had 4 successive undetectable results but my last 2 tests 6 months apart,have shown .035 and .06. I know these are low levels but still concerning. I have an appointment next week with my surgeon, I suspect he will just suggest a wait and see approach. Any harm in being more aggressive and requesting radiation?
Hello Mike, I am still on active surveillance! 17 months of undetectable after RP. My PSA levels to present were 0.1, 0.25, 0.24, and the last was 0.23. I have a PSMA scan on the 9th August! I am still seeing my urologist and in touch with my RO. I believe Dr. Lieb ordered the scan after reading the SPPORT trial results? If my scan is clean and my PSA remains stable, I may chose to continue with active surveillance. TA is certainly the go person for answering your concerns! Please reach out to him!
TA,
I had an RP about 3 years ago and the first 4 scans were undetectacble but the last 2 tests have shown .035 and .06. I saw my surgeon who is at Weill Cornell in NY. He proposed a wait and see approach. The original pathology was a Gleason 7 (3+4) and believed to be organ confined and they tested 8 nodes all negative and the other tissue tested was negative. I know these levels are low but they are above what my previous readings were. I suggested being aggressive and possibly starting radiation at the site of the prostate and understandably the doctor did not want to do this. Are you aware of any other options? I am 54 years old and relatively impatient do the wait and see approach just doesn’t sit well.
Your view would be greatly appreciated.
There is no need for SRT until PSA hits 0.1 or 0.2. There's no advantage to treating sooner.
Thanks. I am meeting with another doctor tomorrow. I am sure he going to say the same thing. Do you have any recommendations for doctors or hospitals? I reached out to the Mayo Clinic but they feel it’s too early. My surgeon doesn’t seem concerned.
Where?
I am in New York City. I currently use Dr. Douglas Scherr at Weill Cornell Presbyterian. I also consult with Dr. David Samadi. I am not opposed to traveling for appointments.
IMO, Samadi is probably the worst urologist (in that he is the least informed) out there. Try Sean McBride at MSK for radiation oncology.
Thank you. Just curious why you feel Samadi is uninformed. I am trying to get an appointment at MSK as well
He may be a good surgeon, but from what he's said publicly, he is not afraid to show how ignorant he is about radiation.
Is he opposed to radiation or is he quick to use radiation?
He's opposed to it as primary therapy. Why are you seeing a urologist now? Do you have urological issues?
Both Scherr and Samadi are urological oncologists. I am going to see the drs at MSK as soon as I can get in to see them but in the interim trying to figure out what is going on with me. I have full urinary function and some impaired sexual function but not changing my quality of life. Should I switch from Scherr and Samadi?
First question: How much do I owe you doc?
Second question: Where can I catch the subway or bus to MSKcc?
Good Luck, Good Health and Good Humor.
j-o-h-n Wednesday 01/12/2022 7:36 PM EST
I surrender... (smiling face here)
Your PSA was 0.1 some day during November last. Now is 0.26. Doubling Time less than 2 months. Very aggressive stuff. PSMA PET has potential for positive detection.