Story so far is that I have been diagnosed with hyperthyroidism/Graves disease. I have been on carbimazole since September. Initial dose was 40mg a day. After 7 weeks I00g of levothyroxine was added in ie block and replace. That only lasted for about 2 and a half weeks as I suspected levo might have triggered some digestive issues. Looks a bit unlikely as digestive issues continued. I have had a separate referral for that and have had a battery of tests from which a working hypothesis of achalasia has been arrived at. In the meantime after stopping the levo I took 20 mg of carbimazole for just over a fortnight reducing to 15mg for the last 11 days. As part of the battery of tests for the digestive issues I had a CT scan of the abdomen which indicated a "lumpiness" in part of the pancreas. As pancreatitis is a known side effect of carbimazole I have requested a change in anti thyroid medication to PTU. I will be speaking with my endo consultant (private not NHS) shortly but any thoughts on PTU and/or my test results would be appreciated. Results above- most recent at the top
Any thoughts on my most recent blood tests - Thyroid UK
Any thoughts on my most recent blood tests
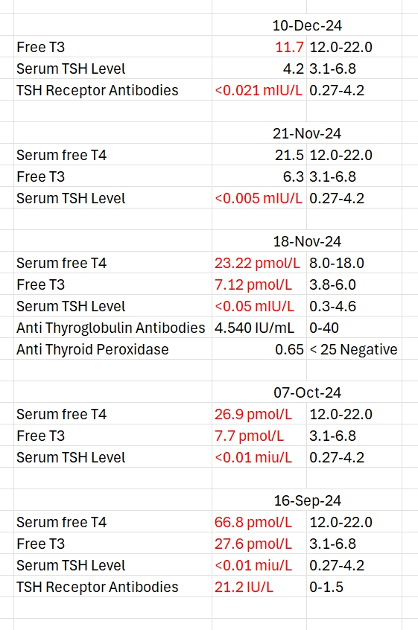
Could you check your results & ranges for last (10/12) test.
I think you may have mixed up results & ranges.
TSH & FT4 result looks hypothyroid. So a decrease in anti-thyroid or increase in replacement required.
Difficult to judge when adjusting doses.
Antibodies have a (0-x) off <x range. The TRab results written currently would be negative.
Have you had gluten screen test?
Serum free T4 11.7 Range 12-22
Free T3 4.2 Range 3.1-6.8
TSH 0.021 Range 0.27-4.2
Sorry I was cutting and pasting in a hurry .... Most recent test result should be as above. I haven't been tested for gluten. All of my digestive issues are upper GI and my gastro consultant thinks are down to essentially a mechanical fault ie achalasia meaning food is sitting in my food pipe too long rather than progressing to the stomach. That diagnosis was on the basis of a CT scan and confirmed with a barium swallow test yesterday. I have a manometry test next week which will give absolute confirmation.
I am not sure how to edit the original post. If you can point me in the right direction I will correct the table
FT4 below range. You may need a lower anti thyroid dose yet but with recent adjustment it’s hard to predict.
PTU is 10x equivalent to carbimazole. If taking 15mg carbimazole you’ll need 150mg PTU. PTU comes in 50mg pills.
Do you have a TRab test result & range?
You can edit posts & replies by going to more & edit. Images can also be deleted & readded. (think you already figured out👍)
I have now spoken to my endocrinologist and he has prescribed 2 x 50mg daily for 3 weeks then blood tests and a further review with a view to halving the dose again.
Is TRab the TSH receptor antibody one. If so the only one I've had is on 16 Sept when it was 21.2 (range 0-1.5). Would it be worth having this done again with my next blood tests?
Thank you
I have now spoken to my endocrinologist and he has prescribed 2 x 50mg daily for 3 weeks
Prescription for what ……PTU or levothyroxine?
PTU. I don't take any levothyroxine now. Treatment plan is now titration of anti thyroid meds, not block and replace.
That’s what I thought but it wasn’t obvious from your reply
Is that a small reduction in dose in comparison to Carbimazole
Because currently Ft4 and Ft3 are both low
Yes it's the equivalent of going from 15mg of carbimazole to 10mg of carbimazole. I agree FT3 and FT4 are low but because I'm waiting for the prescription of PTU to arrive (suspect it will be Monday) I'll have a few days break from any AT meds as we agreed I should stop the carbimazole immediately. I don't have any particular hypothyroid symptoms so hoping levels don't go any lower and creep up a bit with the combination of a few days break and a lower dose. I've also got a medichecks test kit to hand so if necessary can do an earlier test and reduce my dosage if I think I've gone too low.
I haven't been tested for gluten. All of my digestive issues are upper GI and my gastro consultant thinks are down to essentially a mechanical fault ie achalasia meaning food is sitting in my food pipe too long rather than progressing to the stomach.
Gut issues are EXTREMELY common when hypothyroid, resulting in low stomach acid, acid reflux and slow gut function
it’s also VERY common to develop gluten intolerance with Graves’ disease or Hashimoto’s as both are autoimmune
A strictly gluten free diet helps or is essential due to gluten intolerance (no test available) or due to leaky gut and gluten causing molecular mimicry (see Amy Myers link)
Changing to a strictly gluten free diet may help reduce symptoms, help gut heal and may slowly lower TPO antibodies
While still eating high gluten diet ask GP for coeliac blood test first as per NICE Guidelines
nice.org.uk/guidance/ng20/c...
Or buy a test online, about £20
Assuming test is negative you can immediately go on strictly gluten free diet
(If test is positive you will need to remain on high gluten diet until endoscopy, maximum 6 weeks wait officially)
Trying gluten free diet for 3-6 months. If no noticeable improvement then reintroduce gluten and see if symptoms get worse
chriskresser.com/the-gluten...
amymyersmd.com/2018/04/3-re...
Thank you. However I am under a gastro consultant for my gut issues which appear to be a mechanical issue with the working of the esophageal muscles and LES. This is on the basis of a trans nasal gastroscopy, CT scan and barium swallow - all fast tracked. I also have a manometry test to come. All my issues are in the upper GI tract and the provisional diagnosis is achalasia. There may be some food intolerance there and I will certainly discuss with my consultant but I need to get the primary problem which is actually getting any food to as far as my stomach sorted before I look at going gluten free. The sight of my very distended food pipe with a teeny tiny junction at the stomach end and watching what happens when the barium goes down definitely looks more like a mechanical issue.
results on Dec 10th
Ft4 is 11 (12-22) (not Ft3 as you have written)
So Ft4 is below range
You very likely need dose reduction in Carbimazole
Or go back on (slightly reduced) dose levothyroxine
No he doesn't seem bothered by the TSH only FT3 and FT4. And although she's not responsible for managing my hyperthyroidism my GP also concurred that TSH is the last thing to resolve and doesn't seem overly concerned with it.
He's not perfect 😅 I've had to change to PTU because there is a question mark over whether carbimazole has triggered something in my pancreas. He started from the standpoint that of course it couldn't but then when he'd done some digging he conceded that I might just have a point lol
Thank you. You've echoed my thoughts exactly! Trouble with doctors is I don't think they want to acknowledge side effects because they think you'll stop taking whatever it is. Hardly informed consent! And whilst my digestive woes do seem to be a separate condition I find it interesting that they started 7 weeks after I started carbimazole so still within a timespan where carbimazole could be the trigger. Other than being overdosed how did you find PTU?
Very interesting story but scary the ignorance of so called experts. If only all doctors were like my gastro consultant. She's young but has a lovely way with patients and most importantly she listens! Why can't doctors understand that whilst patients might not be medically qualified we are the people who've lived in the body they are treating and we know what feels off!