hi my daughter is taking 125 Levothyroxine but is still feeling unwell. Fatigue, unable to lose weight and hair loss. These are her latest bloods. Could she be feeling unwell being on too much levo?
Many thanks
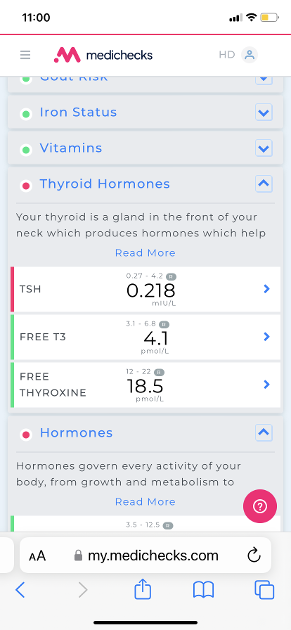
hi my daughter is taking 125 Levothyroxine but is still feeling unwell. Fatigue, unable to lose weight and hair loss. These are her latest bloods. Could she be feeling unwell being on too much levo?
Many thanks
I think not enough FT3 low in ratio to FT4.
Poor conversion from FT4 to FT3, most people aim for FT3 near the top of the range. I doubt you will be able to manage that on T4 levothyroxine alone. RT3 is probably quite high as well.
As the reason for poor conversion then there could be multiple issues. The good people on this forum are much better placed to advise, but a genetic defect like DI02 is normally a major player in poor conversion.
I don't think I would be increasing my dose beyond 125mcg if your daughter is still getting hypo symptoms.
Would be good if you were to add her iron and vit results too to give a broader picture
Hello Britt:
The accepted conversion ratio once the T4 is up in the top quadrant of its range is said to be :-
1 / 3.50-4.50 with most people feeling at their best when they come in this ratio at 4 or under :
So if I divide her T4 @ 18.50 by her T3 @ 4.10 I'm getting her conversion of the T4 into T3 which is the actie hormone that runs the brain & body coming in at 4.51 - showing her slightly wide of what is seen as an ok good conversion.
Currently her T4 is at just around 65% through its range and we generally feel best once the T4 is up in the top quadrant at around 80% with the T3 tracking just behind at around 70% :
Conversion of T4 into T3 can be compromised by non optimal levels of core strength vitamins and minerals -
can you please tap in the ferritin, folate, B12 and vitamin D results - along with the inflammation and antibody readings and ranges - and down regulation of thyroid hormones can also be because of any physiological stress ( physical or emotional) depression dieting and ageing.
Her TSH is quite low but would try and encourage a dose increase so her T4 reaches the top quadrant where we may see a much healthier T3 as it is too low a level of T3 that causes the symptoms likely being tolerated.
Is your daughter dealing a thyroid AI disease - I think I've seen your posts before but never read them so apologise if you have already shared this information.
Hi thanks for your reply. These are her results
Ok - so both her thyroid antibody readings are positive and over range -
so your daughter is dealing with Hashimoto's - a thyroid auto immune health issue that expresses itself with erratic ' own swings ' in thyroid hormone production and levels as this AI disease systematically attacks the thyroid - but these ' swings ' are transient but leave the patient dealing with various symptoms / degrees of hypothyroidism and likely given enough time needing more than just T4 monotherapy thyroid hormone replacement.
I think we are still missing the inflammation marker CRP and ferritin result ?
I read many dealing with Hashimoto's need to have to ' heal their gut ' as they can have issues caused by certain food stuffs - so it will be sensible to get checked out for food intolerance to gluten, dairy, wheat while eating her chosen food stuffs just to rule in or out these issues -
Many forum members follow the advice and research of Izabella Wentz who writes as thyroidpharmacist.com
Thank you for your reply.
Thanks - well here we have a big part of the problem as I'm reading her ferritin is only at 36 and this is much too low, though in the range, and likely a major cause of her continued symptoms of hypothyroidism.
I started researching ferritin when mine came in at 22 - and I read in several well respected articles that no thyroid hormone replacement works well until ferritin is at least over 70 -
I now aim to maintain ferritin at around 100 - folate around 20 active B12 125 ( serum B12 500++ ) and vitamin D at around 125.
Would you mind letting me know what supplements you you take please
I'm now able to maintain my ferritin through food by eating 1 tub of frozen chicken livers a week - which I can now, only find in Waitrose.
I found the NHS iron supplements too harsh on my stomach and wasn't offered any alternatives so purchased Gentle Iron and took 3 capsules a day - and on reflection -
any iron bisglycinate OTC preparation will be better tolerated than those prescribed - I also ate liver twice a week and drank Spatone Iron sachets daily x 4 sachets -
I also made sure that I also put some acid cider vinegar into my stomach before eating my main meal of the day containing the most protein so to enable me to better breakdown and extract key nutrients from food.
Many of us have low stomach acid - and there is a ' burp test ' on youtube worth watching and testing for yourself - and if you are slow to burp - you likely need just a teaspooon full of ACV with the ' mother enzyme ' in some water to drink before the main meal of the day.
As for now - I am on maintenance doses and take daily take 1 x Ingennus Super B complex with folate tablet + 1 x Doctors Best D3 x 5000 iu + Healthy Origins vitamin K2 - MK7 which are both suspended in capsule form with extra virgin olive oil.
Free T4 (fT4) 18.5 pmol/L (12 - 22) 65.0%
Free T3 (fT3) 4.1 pmol/L (3.1 - 6.8) 27.0%
Was test done early morning, ideally before 9am, only drinking water between waking and test and last dose levothyroxine 24 hours before test
Does she always get same brand levothyroxine at each prescription
Ft3 is low……therefore vitamin levels likely poor
Exactly what vitamin supplements is she taking
ESSENTIAL to test vitamin D, folate, B12 and ferritin at least annually
Please add most recent results
Hairloss suggests low iron/ferritin
Is her hypothyroidism autoimmune
Is she on gluten free and/or dairy free diet
If not GF get coeliac blood test via GP BEFORE trialing for 3-6 months minimum
Hi, yes she did her test as advised on this forum.
She has had coeliac test which was negative. Her condition is autoimmune . These are some of her other results, thank you for taking the time to reply
Ferritin result?
How much vitamin D is she taking
Also taking magnesium?
Is she taking daily vitamin B complex?
B12 and folate look reasonable
IMPORTANT......If you are taking vitamin B complex, or any supplements containing biotin, remember to stop these 5-7 days before ALL BLOOD TESTS , as biotin can falsely affect test results
endo.confex.com/endo/2016en...
endocrinenews.endocrine.org...
In week before blood test, when you stop vitamin B complex, you might want to consider taking a separate folate supplement (eg Jarrow methyl folate 400mcg)
She has had coeliac test which was negative. Her condition is autoimmune .
Autoimmune thyroid disease - Hashimoto's affects the gut and leads to low stomach acid and then low vitamin levels
Low vitamin levels affect Thyroid hormone working
Poor gut function can lead leaky gut (literally holes in gut wall) this can cause food intolerances and inflammation
Most common by far is gluten.
Dairy is second most common.
A trial of strictly gluten free diet is always worth doing
Only 5% of Hashimoto’s patients test positive for coeliac but a further 81% of Hashimoto’s patients who try gluten free diet find noticeable or significant improvement or find it’s essential
A strictly gluten free diet helps or is essential due to gluten intolerance (no test available) or due to leaky gut and gluten causing molecular mimicry (see Amy Myers link)
Changing to a strictly gluten free diet may help reduce symptoms, help gut heal and may slowly lower TPO antibodies
As her test is negative recommend trialing strictly gluten free diet
Trying gluten free diet for 3-6 months. If no noticeable improvement then reintroduce gluten and see if symptoms get worse
chriskresser.com/the-gluten...
amymyersmd.com/2018/04/3-re...
thyroidpharmacist.com/artic...
drknews.com/changing-your-d...
Non Coeliac Gluten sensitivity (NCGS) and autoimmune disease
pubmed.ncbi.nlm.nih.gov/296...
The predominance of Hashimoto thyroiditis represents an interesting finding, since it has been indirectly confirmed by an Italian study, showing that autoimmune thyroid disease is a risk factor for the evolution towards NCGS in a group of patients with minimal duodenal inflammation. On these bases, an autoimmune stigma in NCGS is strongly supported
nuclmed.gr/wp/wp-content/up...
In summary, whereas it is not yet clear whether a gluten free diet can prevent autoimmune diseases, it is worth mentioning that HT patients with or without CD benefit from a diet low in gluten as far as the progression and the potential disease complications are concerned
restartmed.com/hashimotos-g...
Despite the fact that 5-10% of patients have Celiac disease, in my experience and in the experience of many other physicians, at least 80% + of patients with Hashimoto's who go gluten-free notice a reduction in their symptoms almost immediately.
Similarly few months later consider trying dairy free too. Approx 50-60% find dairy free beneficial
With loads of vegan dairy alternatives these days it’s not as difficult as in the past
Dairy free can help with weight issues too
Post discussing gluten
healthunlocked.com/thyroidu...
Recent research in China into food intolerances with Hashimoto’s
healthunlocked.com/thyroidu...
Thank you so much. I will discuss gluten free and diary free too. Would you consider adding T3?
I would
A) increase Levo and ensure always same brand
B) improve vitamin levels
C) trial GF/DF
Retest thyroid levels again in another 2-3 months after this
Assuming Ft3 remains low ……then consider getting T3 prescribed alongside Levo
Here’s link for how to request Thyroid U.K.list of private Doctors emailed to you, but within the email a link to download list of recommended thyroid specialist endocrinologists who will prescribe T3
Ideally choose an endocrinologist to see privately initially and who also does NHS consultations so that might eventually transfer to getting T3 on NHS
thyroiduk.org/contact-us/ge...
Thank you so much for your advice
Is she taking Vitamin B complex?
I just checked top of folate range on Medichecks is 60 ….so her folate is on low side
So suggest a daily vitamin B complex
supplementing a good quality daily vitamin B complex, one with folate in (not folic acid)
This can help keep all B vitamins in balance and will help improve B12 levels too
Difference between folate and folic acid
healthline.com/nutrition/fo...
Many Hashimoto’s patients have MTHFR gene variation and can have trouble processing folic acid supplements
thyroidpharmacist.com/artic...
B vitamins best taken after breakfast
Igennus B complex popular option. Nice small tablets. Most people only find they need one per day. But a few people find it’s not high enough dose and may need separate methyl folate couple times a week
Post discussing different B complex
healthunlocked.com/thyroidu...
Thorne Basic B recommended vitamin B complex that contains folate, but they are large capsules. (You can tip powder out if can’t swallow capsule) Thorne can be difficult to find at reasonable price, should be around £20-£25. iherb.com often have in stock. Or try ebay
IMPORTANT......If you are taking vitamin B complex, or any supplements containing biotin, remember to stop these 5-7 days before ALL BLOOD TESTS , as biotin can falsely affect test results
endo.confex.com/endo/2016en...
endocrinenews.endocrine.org...
In week before blood test, when you stop vitamin B complex, you might want to consider taking a separate folate supplement (eg Jarrow methyl folate 400mcg)
Post discussing how biotin can affect test results
healthunlocked.com/thyroidu...
FT3 is the most important result followed by FT4.
FT4. 18.5 (12 - 22) is 65% through the ref range
FT3. 4.1 ( 3.1 -6.8) is 27.3% through the ref range
We aim to have both Frees approaching 75% through the ref range
High FT4 with low FT3 = poor T4 to T3 conversion
Her dose is 125mcg levo
Initially an increase to 150mcg should start to raise FT3
It looks as if she might find a later increase to 175mcg helpful....she has room in the FT4 ref range to do this.
If these 2 increases don't raise FT3 adequately to resolve symptoms then it's time to introduce a little T3.....via an endocrinologist....referrel from GP.
Conversion can be impaired by the Dio2 polymorphism especially if it is inherited from both parents ( homozygous) but proven to be much less so if inherited from only one parent (heterozygous)
Using the FT4/FT3 comparison is quicker and cheaper. However a naysaying endo may be more easily persuaded to prescribe T3 based on evidence of a polymorphism
We aim to raise FT3 by first increasing levo before jumping straight to T3....it is less of a "fight" and a faff!!
Low T3 causes slow metabolism which calories are not being adequately burned, the result being weight gain....a very common hypo symptom. And low energy.
It is also vital to optimise vit D, vit B12, folate and ferritin to support thyroid function
Have these been tested recently?
TSH is not a reliable marker but used as a guide should be 1 or under. TSH focussed medics probably, wrongly, consider her results are "normal"....or even wrongly suggest her labs show overmedication. Beware!
Two years ago her thyroid antibodies were high indicating thyroid autoimmune disease/ Hashimoto's. Is her diet gluten free to help symptoms?
But SlowDragon has already given you excellent advice re this
So, yes, she is undermedicated and initially needs more levo.
She should consult her GP who hopefully understands thyroid hormones....many do not.
Good luck!
Also note that ferritin does not have a direct role in the synthesis or processing of thyroid hormones. Therefore there is no minimum threshold for our ferritin results required for thyroid hormone replacement to work. pennyannie
Ferritin is an indicator of iron stores in the body and plays a role in iron metabolism, and of course iron is essential for everyone including us, but it does not directly interact with thyroid hormone pathways.
I have had ferritin between 5 and 25 for 2 years and have had almost all my symptoms alleviated by optimizing my t4/t3 levels.
Of all the direct and indirect measures of iron to look at for minimum threshold for thyroid hormone replacement to work - the best is transferrin saturation percent.
That needs to be a minimum of 30% and optimally 35-45% for t3 to work at the cellular level, and no higher to avoid iron toxicity.
That being said, no one measure of iron is sufficient, they all need to be looked at together when managing our iron profile.
You should not be supplementing iron with those results, instead increase iron rich foods and absorption helpers like Vit c if it’s a non-animal source.
I stand by what I have written - with a slowed metabolism it will take some time to build up ferritin stores through just eating iron rich foods and having ' been there myself ' know how much improved I was once my ferritin was supplemented much higher in the range -
An iron panel makes sense and in UK this would likely have been run when the reading was below 30 as this is the ' cut off ' number when iron deficient anemia is diagnosed and further investigations are automatically carried out.
I don't doubt and wrote that the O/P needs a dose increase in T4 and eventually a trial of T3 to restore these two vital hormones - but in the UK T3 is not readily prescribed on the NHS - and with primary care working on just TSH readings - for some, even getting an increase in T4 is difficult.
And all this takes time and I can't see the point of not supplementing ferritin since the level is low and the patient symptoms those we see when ferritin is low in the range.
This is my concern. Her GP would say she’s over medicated based on her tsh level
I too agree with every word you wrote in practice. That low ferritin on its own causes symptoms AND is also a reflection of overall iron health.
My point was just root cause analysis.
In our bloods and body the level of ferritin is not the root cause of how well our body uses thyroid hormones. Of course optimal iron improves thyroid pathways. And ferritin improves iron.
But at a cellular level there are a few steps in between. That’s the main point I’m making.
So whereas ferritin is importantly both on its own and as an indicator of other iron measures, one can have low ferritin and thyroid hormone pathways that work.
Transferrin saturation percent, on the other hand, when not at a minimum threshold actually indicates that at the cellular level our t3 actually won’t have enough of the iron it needs to get where it needs to go and work.
I think we are in practice saying the same thing - but although we all need to get ferritin up towards 100 for optimal health, it’s not a minimum threshold like a tsat% is for example.
Also - there is no way to supplement ferritin. One can only supplement and increase iron to optimal, and as a derivative, ferritin will increase.
Yes I guess so - the issue is in the Uk - we are generally under medicated and dosed and monitored on just TSH readings - which as we know is a very unreliable measure of anything oce on any form of thyroid hormone replacement -
T4 is the only treatment option in primary care and if in the range somewhere - some doctors see this as ' job done ' - primary care doctors haven't detailed blood tests and rarely have no idea about T3/T4 conversion - and can't do much about it anyway as they can't instigate T3 prescriptions any longer.
So - left with a slowed metabolism it is harder to extract key nutrients through food - which in theory is ' all we need to do ' and when T3 is well placed in the range and you are metabolising becomes a normal every day function of the body that many can then take for granted.
The O/P was with fatigue and hair loss and we have seen this all too often being a symptom of low ferritin stores - though O/P will be in the NHS range for ferritin and told she's good to go and not offered any supplements on the NHS.
Having been offered iron supplements on the NHS I wouldn't recommend these to anybody anyway - but that's a whole other conversation.
Thank you for the clarification.
Not much better in the US!
We are in total agreement - practically for OP advice is the same between you, me and SD:
With an iron panel like that unfortunately (or fortunately however you look at it) her iron is pretty good… leaving her with the action plan of increasing iron rich foods to bring up the ferritin. Ie, supplementing with those numbers is not recommended.
I am impressed at your being able to eat a tub of chicken livers! I tried and just couldn’t.
BRITT1DENMARK you should indeed increase iron in your diet as much as possible. You can also regularly test your full iron panel. If other measures drop you can consider a careful supplementing plan.
Feel feee to tag me in a few months if you get another iron panel after increasing iron in your diet.
The reason we are so careful with iron is that excess iron in the blood is toxic and causes irreversible damage to our organs and soft tissues over time. Our bodies have no way to excrete excess iron, and so it will accumulate over your lifetime. There is no risk of this when we eat iron rich foods. Just when we supplement.
Let us know how it goes!
I'm not sure I even saw an iron panel as was writing from the ferritin reading -
So - 200 grams a week maximum is just a small tub of frozen chickens livers - defrosted and flash fried down in a matter on minutes in extra virgin olive oil - I then whizz down into a mush - some might call a pate - and keep it in the fridge in an old jamjar and take around a spoonful a day - helped down with a dollop of Helmans - and my Mary Poppins solution to not having to need the medicine to go down.
It’s on my shopping list 😄
I think initially your daughter needs to build up her ferritin level and suggested an iron bisglycinate supplement - as detailed previously -
My ferritin level is now up and I am able to maintain the level by eating iron rich foods -
and now I self medicate and take NDT my metabolism is running that bit better so my body is better able to breakdown the key nutrients from my food and better able to absorb, utilise and replenish my core strength overnight ready for whatever comes my way the next day.
Impressive. My parents eat pate like it’s going out of style. They eat liverwurst too… yuck lol!
When I did my first round “eat more iron rich foods” I horrified my family by making liver smoothies : ) threw in lots of stuff to mask the taste.
That being said I also believe a dollap of hellmans makes most things better : )
The crazy thing is that 200 grams of chicken liver is about 20 mgs elemental iron. Which is one three arrow capsule…!
Also as a reminder for anyone else reading this reply - you really don’t want your eat more than 150-200 grams of chicken liver a week because you will hit vitamin A levels that are toxic, especially since one gets vitamin A from other food sources.
I read a fascinating article on polar bears that drive that point home. In fact, the livers of polar bears, seals, and other arctic animals contain such high concentrations of vitamin A that eating them is dangerous for humans. Early Arctic explorers even learned to avoid polar bear liver after suffering toxicity symptoms. An interesting example of evolutionary adaptation to extreme diets in specific environments!
Darned if you do, darned if you don’t!
Ferritin under 50
she needs to improve her very low ferritin by increasing iron rich foods in her diet
Possibly small dose iron supplement
cks.nice.org.uk/topics/anae...
Serum ferritin level is the biochemical test, which most reliably correlates with relative total body iron stores. In all people, a serum ferritin level of less than 30 micrograms/L confirms the diagnosis of iron deficiency
Never supplement iron without doing full iron panel test for anaemia first and retest 3-4 times a year if self supplementing.
It’s possible to have low ferritin but high iron
Test early morning, only water to drink between waking and test. Avoid high iron rich dinner night before test
If taking any iron supplements stop 5-7 days before testing
Medichecks iron panel test
medichecks.com/products/iro...
Look at increasing iron rich foods in diet
Eating iron rich foods like liver or liver pate once a week plus other red meat, pumpkin seeds and dark chocolate, plus daily orange juice or other vitamin C rich drink can help improve iron absorption
List of iron rich foods
Links about iron and ferritin
irondisorders.org/too-littl...
davidg170.sg-host.com/wp-co...
Great in-depth article on low ferritin
oatext.com/iron-deficiency-...
drhedberg.com/ferritin-hypo...
This is interesting because I have noticed that many patients with Hashimoto’s disease and hypothyroidism, start to feel worse when their ferritin drops below 80 and usually there is hair loss when it drops below 50.
healthunlocked.com/thyroidu...
Posts discussing Three Arrows as very effective supplement
Great replies from @FallingInReverse
re ferritin and Three arrows
healthunlocked.com/thyroidu......
healthunlocked.com/thyroidu...
healthunlocked.com/thyroidu...
Great reply by @fallinginreverse
healthunlocked.com/thyroidu...
Ferrodyn supplement
healthunlocked.com/thyroidu...
Iron patches
healthunlocked.com/thyroidu...
Thyroid disease is as much about optimising vitamins as thyroid hormones
healthunlocked.com/thyroidu...
restartmed.com/hypothyroidi...
Post discussing just how long it can take to raise low ferritin
healthunlocked.com/thyroidu...
Iron and thyroid link
healthunlocked.com/thyroidu...
Posts discussing why important to do full iron panel test
healthunlocked.com/thyroidu...
Good iron but low ferritin
healthunlocked.com/thyroidu...
healthunlocked.com/thyroidu...
healthunlocked.com/thyroidu...
Chicken livers if iron is good, but ferritin low
healthunlocked.com/thyroidu...
Shellfish and Mussels are excellent source of iron
healthline.com/nutrition/he...
Iron deficiency without anaemia
healthunlocked.com/thyroidu...
Ferritin over 100 to alleviate symptoms
healthunlocked.com/thyroidu...
healthunlocked.com/thyroidu...
Great research article discussing similar…..ferritin over 100 often necessary
ncbi.nlm.nih.gov/pmc/articl...
Low Iron implicated in hypothyroidism
healthunlocked.com/thyroidu...
Really interesting talk on YouTube, link in reply by Humanbean discussing both iron deficiency and towards end how inflammation can also be an issue
healthunlocked.com/thyroidu...
Inflammation affecting ferritin
healthunlocked.com/thyroidu...
Updated reference ranges for top of ferritin range depending upon age
healthunlocked.com/thyroidu...
Thank you for your incredible patience while you have been awaiting the outcome of our ferritin reference range review. We conducted this with Inuvi lab, which has now changed the reference ranges to the following:
Females 18 ≤ age < 40. 30 to 180
Females 40 ≤ age < 50. 30 to 207
Females 50 ≤ age < 60. 30 to 264l
Females Age ≥ 60. 30 to 332
Males 18 ≤ age < 40 30 to 442
Males Age ≥ 40 30 to 518
The lower limits of 30 are by the NICE threshold of <30 for iron deficiency. Our review of Medichecks data has determined the upper limits. This retrospective study used a large dataset of blood test results from 25,425 healthy participants aged 18 to 97 over seven years. This is the most extensive study on ferritin reference ranges, and we hope to achieve journal publication so that these ranges can be applied more widely.