Bisoprolol stopped my thyroxine from working
bisoprolol stopped my thyroxine from working - Thyroid UK
bisoprolol stopped my thyroxine from working
No, it didn't stop your levo from working, it reduced your body's ability to convert T4 (levo) to T3.
I feel terrible what can I do doctor doesn’t understand I’m slowly going downhill since January when I started and my heart rhythmn is shocking bi had a total thyroidectomyb29 years ago but I really feel shocking since I was given betablockers I’ve had atenolol then carvedilol now bisoprolol and symptoms are all the samec
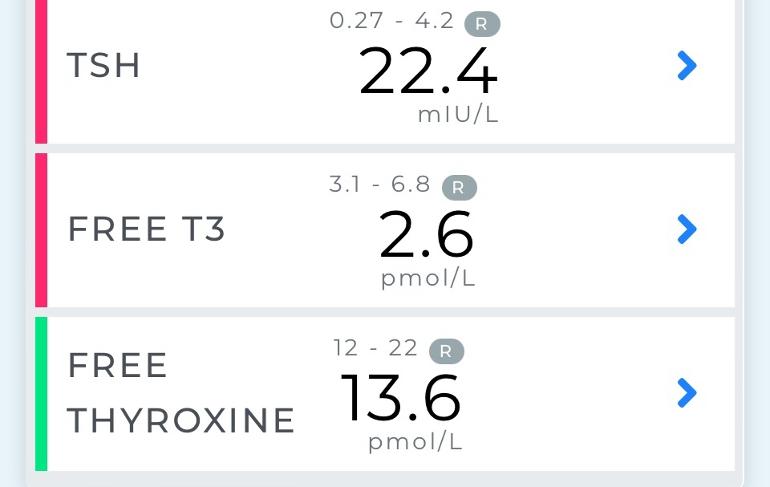
There are other things he could give you that don't have that effect. Show him your blood test results, with that very low FT3 - that's what's making you feel bad. It's a well-known effect of some beta-blockers, he should know that.
Why are you taking beta-blockers?
High blood pressure and tachycardia I gave him my bloods and he said just increase thyroxine by 25, they wouldn’t test my t3 I paid for it as I feel so ill and after all these years of no gland I know when it’s out
Yes, of course you know. But, do you know that high blood pressure and tachycardia can be symptoms of hypo? And I should imagine your FT3 is always pretty low. So that could be what's causing it and you don't really need Beta Blockers anyway. Could be. 
I’m at a loss as what to do next to get my t3 up I asked doc if I could stop beta blockers and he said no it’s dangerous to just stop them as my blood pressure will spike
I suppose I will have to wean off beta blockers I’m already taking half a 1.25 as my pulse keeps dropping too low he halved it then increased levo by 25 but said I will have to get my own t3 checked again in a month in all the years with no gland I have never felt so poorly
My understanding is that bisoprolol doesn't affect hormone conversion, because it's selective, but propranolol does affect. Been on both. I'd say you just need to keep increasing your thyroid meds.
I was on carvedilol before I only switched to bisoprolol 2 weeks ago
Opinions differ. Some people say that all Beta Blockers affect conversion. Perhaps it depends on the person, like most things thyroid. I've only taken them once and I was on T3 mono-therapy at the time, so I have not personel experience. But, the fact is the OP's FT3 is below range, and that's what's making her ill. 
I had this problem when I was given Bisoprolol (Diagnosed with Paroxysmal aFib) and told to take it in the morning. The Betablocker and my Thyroxine(T4 and T3) together resulted in dropped FT3 and FT4 Levels. I now take the Bisoprolol at night and Thyroxine in the morning which seems to work ok. My TSH didn’t go up so high like yours though.
No, it didn’t, but my side effects did not go away after the initial ’settling in’ period, as I was told by doctors but are increasing and I am seeing an EP (Electrophysiologist, private) to see if there is an alternative for bisoprolol or beta blockers in general.
My side effects are debilitating nausea, anxiety, wild dreams, and gastrointestinal problems. Also feel breathless when trying to increase my activity level sharply, feels like a delayed body reaction to it, which of course is what these drugs do- they block the uptake of adrenaline.
Would rather not take them but they have kept my heart rate more stable and I have a lover pulse.
It seems we all react differently to these drugs
my doctor has stopped bisoprolol due to heart rate going too low and blood pressure keep spiking hits 180/130 from very early morning so they have stopped bisoprolol and replaced it with losartan 25 mg I’m starting to feel very anxious I have to see doc in 1 week
Just seen these nhs bloods out of range but doc never mentioned
Mch25.3 (27-32)
Mcv81 .4(80-32)
Mchc 311(320-370)
Haemoglobin 136G/L(115-165)
Haemocrit0.437L/L(0.37-0.48)
Rbc 5.37 10 9/L(3.80-5.80)
WBC 13.01 10 9/L (4.011.0)H
Also RDW 15.1% H(12-15)
Nobody mentioned these do I need to take supplements
A high Red Cell Distribution Width can occur in several circumstances.
It means that instead of your RBCs being of similar size, the sizes are more spread out - often having more small ones and more big ones.
A typical cause of small RBC is iron deficiency. A typical cause of large RBC is vitamin B12 (and/or folate) deficiency. When you have both, RDW tends to rise even more. I note your Mean Cell Volume is also high - which tends to point at B12/folate. But your MCH and MCHC are also low-ish and you might well also need iron.
However, RDW also changes if you change your circumstances. For example, if you start or stop iron, B12 or folate supplementation.
In hypothyroidism, absorption of B12 is often impaired. It would be good to get B12 and folate tested, if possible. And, depending on results, start B12 first, then folate supplementation.
Did they not test ferritin?
Mcv was normal 81.4(80-102) it was mch and Mchc low. No they didn’t test ferritin. Also I eat plenty iron so mustn’t be absorbing do you think
MCV was very near the bottom of the reference interval - I would not call that "normal". Most especially because it being low reinforces the message of the other test results. You are low in iron.
In what form(s) are you consuming plenty of iron? Yes, it could well be that you are not absorbing it adequately.
This is a link to a very good article in the British Medical Journal discussing what the 'normal range' really is. Very readable.
The normal range: it is not normal and it is not a range
MCV is Mean Cell (or Corpuscular) Volume. Your low in range MCV is telling you that the average size of your red blood cells is low i.e. they are smaller than desirable. Small (or large) red blood cells are not as good at carrying oxygen as they should be. Ideally your MCV should be close to the middle of the range.
Ferritin is a measure of your iron stores.
Low in range or under range MCV happens when people are low in iron and/or ferritin.
High in range or over range MCV happens when people are low in B12 and/or folate.
If you are low in one or both B12 and folate AND low in one or both serum iron and ferritin then the result of an MCV test could be anywhere in range and isn't likely to be informative. In this case the only way to determine what is affecting your MCV is to get your serum iron, ferritin, B12, and folate tested separately.
A lot of people have problems with iron/ferritin because they absorb it poorly, even though they might eat a diet high in iron. The other common problem with iron and ferritin is that for some people it can take a long, long time to raise.
a lower pulse rate, of course!