hi, I went private regarding my thyroid nearly a year ago now. Before going to this private thyroid clinic I was on 50 mg of levothyroxine. I suffered from gastro problems, constant reflux, burning stomach, constipation. Also severe coldness, tiredness. After checking my levels the private doctor put me on one and a half grains of armour NDT. Following bloods every 3 months I’ve now worked my way up to 2.5 grains. constipation is gone, coldness and tiredness are gone but my reflux and burning stomach remain. These were always my most debilitating symptoms as I struggle to eat many foods or drink anything but water or tea. I’ve managed to put on some weight and I’m bac at work but because of y gastro problems I have next to no social life which rest gets me down. Are my gastro problems maybe not related to my thyroid? Is their still room for upping my dose? Is it a vitamin or mineral problem? I’ll post my latest results. I’ve recently had a 300000iu vit d injection as I could see that my levels were low and I can’t stomach the vit d oral supplements. Any advice as always would be greatly appreciated. Thanks
still have stomach issues: hi, I went private... - Thyroid UK
still have stomach issues
Hi Bigfraz
Welcome to the forum
Yes please do gather your blood tests and pop them on with the ranges (numbers in brackets) and make sure to keep them anonymous. 😊👍 Some of your hypo symptoms have been resolved so how are you feeling over all?
Give us some background to your general health anything else health related. It all helps to build a picture. We advise from a place of lived experience, none of us have been medically trained. Where abouts are you are you in the UK?
We can have gut issues and checking and supplementing to get the vitamins optimal (not just scraping along the bottom of the range ) is very important.
Many people suffering from hypothyroidism have low stomach acid. It presents as heartburn just like high stomach acid but being treated with proton pump inhibitors PPI’s only make things worse. I had gut issues at the start, many of us do.
Changing diet can help. If you look at SlowDragon ’s profile (click on her icon) and go to replies you will be able to find loads of information on vitamins and testing. She is a legend 🤗
If you click on my face you will see my back story in my bio. Reading lived experience is a really valuable inroad to starting to get to grips with your own condition. We are all different and our routes back to health differ, the only common thread seems to be the battle to get there.
Thanks for your reply, Charlie. I’ve posted my most recent results in my queries. I suspect low stomach acid is causing my symptoms. Gastro problems aside everything else sees to have resolved, or greatly improved
Here's some links about low stomach acid. The technical name is 'hypochlorhydria', so you can google for that. Unfortunately most doctors don't know about it and it's not on the main NHS website - I've looked. I hope these are helpful.
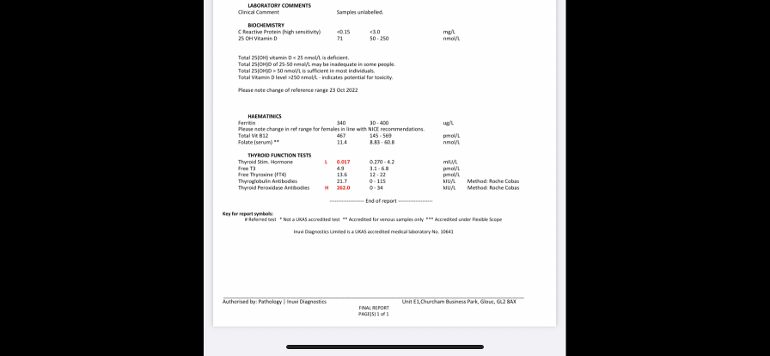
Can you repost the image in comments or type the results out. Its pretty illegible at the moment.
Welcome to the forum
What vitamin supplements are you currently taking
Vitamin D 71
How low was vitamin D before injection
Frequently get improvements when vitamin D is maintained at least over 100nmol. Aiming for 100-150nmol
Have you tried Better You vitamin D mouth spray
Absorbed in mouth so avoids gut issues
B12 467
Better at least over 500
Folate 11.4 (8-60)
So obviously far too low
Will add separate replies on vitamin details
Ferritin 340
good
High TPO antibodies confirms autoimmune thyroid disease aka Hashimoto’s
Have you had coeliac blood test
If not get tested BEFORE trialing strictly gluten free diet
My vit d levels you can see are before injection. I see my folate is low. Tested negative for coeliac. Going by my levels do you think I need more NDT?
Thanks
So I would retest vitamin D now
NHS easy postal kit vitamin D test £31 via
Consider taking 2000iu daily vitamin D mouth spray daily to maintain good level
You might need higher dose, especially in winter…. than summer
Every person is different as to how much they need
Some are fine on 1000iu daily……others might need 4000-5000iu daily as maintenance dose
Test twice yearly, especially while working out what dose you personally need
Low B12 and low folate
Low B12 symptoms
b12deficiency.info/signs-an...
methyl-life.com/blogs/defic...
With serum B12 result below 500, (Or active B12 below 70) recommended to be taking a separate B12 supplement and about a week later add a separate vitamin B Complex
Then once your serum B12 is over 500 (or Active B12 level has reached 70), you should be able to reduce then stop the B12 and just carry on with the B Complex.
If Vegetarian or vegan likely to need ongoing separate B12 few times a week
B12 drops
natureprovides.com/products...
Or
B12 sublingual lozenges
uk.iherb.com/pr/jarrow-form...
cytoplan.co.uk/shop-by-prod...
B12 range in U.K. is too wide
Interesting that in this research B12 below 400 is considered inadequate
healthunlocked.com/thyroidu...
Low folate
supplementing a good quality daily vitamin B complex, one with folate in (not folic acid)
This can help keep all B vitamins in balance and will help improve B12 levels too
Difference between folate and folic acid
healthline.com/nutrition/fo...
Many Hashimoto’s patients have MTHFR gene variation and can have trouble processing folic acid.
thyroidpharmacist.com/artic...
B vitamins best taken after breakfast
Thorne Basic B recommended vitamin B complex that contains folate, but they are large capsules. (You can tip powder out if can’t swallow capsule)
Thorne currently difficult to find at reasonable price, should be around £20-£25. iherb.com often have in stock. Or try ebay
Other options
healthunlocked.com/thyroidu....
Igennus B complex popular option too. Nice small tablets. Most people only find they need one per day. But a few people find it’s not high enough dose
personally I take Igennus or Thorne on alternate days
IMPORTANT......If you are taking vitamin B complex, or any supplements containing biotin, remember to stop these 7 days before ALL BLOOD TESTS , as biotin can falsely affect test results
endo.confex.com/endo/2016en...
endocrinenews.endocrine.org...
In week before blood test, when you stop vitamin B complex, you might want to consider taking a separate folate supplement (eg Jarrow methyl folate 400mcg) and continue separate B12 until over 500
Post discussing how biotin can affect test results
Vitamin D, magnesium and K2
GP should advise on self supplementing if vitamin D over 50nmol, but under 75nmol (but they rarely do)
mm.wirral.nhs.uk/document_u...
But with Hashimoto’s, improving to at least 100nmol by self supplementing may be better
pubmed.ncbi.nlm.nih.gov/218...
vitamindsociety.org/pdf/Vit...
Once you Improve level, very likely you will need on going maintenance dose to keep it there.
Test twice yearly via NHS private testing service when supplementing
Vitamin D mouth spray by Better You is very effective as it avoids poor gut function.
There’s a version made that also contains vitamin K2 Mk7.
One spray = 1000iu
amazon.co.uk/BetterYou-Dlux...
It’s trial and error what dose we need, with thyroid issues we frequently need higher dose than average
Vitamin D and thyroid disease
grassrootshealth.net/blog/t...
Web links about taking important cofactors - magnesium and Vit K2-MK7
Magnesium best taken in the afternoon or evening, but must be four hours away from levothyroxine
betterbones.com/bone-nutrit...
medicalnewstoday.com/articl...
livescience.com/61866-magne...
sciencedaily.com/releases/2...
Interesting article by Dr Malcolm Kendrick on magnesium
drmalcolmkendrick.org/categ...
Vitamin K2 mk7
Gluten and dairy
Your antibodies are high this is Hashimoto's, (also known by medics here in UK more commonly as autoimmune thyroid disease).
Hashimoto's affects the gut and leads to low stomach acid and then low vitamin levels
Low vitamin levels affect Thyroid hormone working
Poor gut function can lead leaky gut (literally holes in gut wall) this can cause food intolerances.
Most common by far is gluten.
Dairy is second most common.
A trial of strictly gluten free diet is always worth doing
Only 5% of Hashimoto’s patients test positive for coeliac but a further 81% of Hashimoto’s patients who try gluten free diet find noticeable or significant improvement or find it’s essential
A strictly gluten free diet helps or is essential due to gluten intolerance (no test available) or due to leaky gut and gluten causing molecular mimicry (see Amy Myers link)
Changing to a strictly gluten free diet may help reduce symptoms, help gut heal and may slowly lower TPO antibodies
While still eating high gluten diet ask GP for coeliac blood test first or buy test online for under £20, just to rule it out first
Assuming test is negative you can immediately go on strictly gluten free diet
(If test is positive you will need to remain on high gluten diet until endoscopy, maximum 6 weeks wait officially)
Trying gluten free diet for 3-6 months. If no noticeable improvement then reintroduce gluten and see if symptoms get worse
chriskresser.com/the-gluten...
amymyersmd.com/2018/04/3-re...
thyroidpharmacist.com/artic...
drknews.com/changing-your-d...
Non Coeliac Gluten sensitivity (NCGS) and autoimmune disease
pubmed.ncbi.nlm.nih.gov/296...
The predominance of Hashimoto thyroiditis represents an interesting finding, since it has been indirectly confirmed by an Italian study, showing that autoimmune thyroid disease is a risk factor for the evolution towards NCGS in a group of patients with minimal duodenal inflammation. On these bases, an autoimmune stigma in NCGS is strongly supported
nuclmed.gr/wp/wp-content/up...
In summary, whereas it is not yet clear whether a gluten free diet can prevent autoimmune diseases, it is worth mentioning that HT patients with or without CD benefit from a diet low in gluten as far as the progression and the potential disease complications are concerned
restartmed.com/hashimotos-g...
Despite the fact that 5-10% of patients have Celiac disease, in my experience and in the experience of many other physicians, at least 80% + of patients with Hashimoto's who go gluten-free notice a reduction in their symptoms almost immediately.
Similarly few months later consider trying dairy free too. Approx 50-60% find dairy free beneficial
With loads of vegan dairy alternatives these days it’s not as difficult as in the past
Post discussing gluten
Before going to this private thyroid clinic I was on 50 mg of levothyroxine. I suffered from gastro problems, constant reflux, burning stomach, constipation. Also severe coldness, tiredness. After checking my levels the private doctor put me on one and a half grains of armour NDT. Following bloods every 3 months I’ve now worked my way up to 2.5 grains
How long have you been on 2.5 grains
Do you normally split the dose as 2 or 3 doses through the day
all thyroid blood tests early morning, ideally just before 9am, only drink water between waking and test and last dose levothyroxine 24 hours before test
This gives highest TSH, lowest FT4 and most consistent results. (Patient to patient tip)
On NDT or T3 - day before test split T3 as 2 or 3 smaller doses spread through the day with last dose 8-12 hours before test
Is this how you did test ?
Depending on timings depends on wether you have room for dose increase
GP was completely incorrect to leave you on only 50mcg levothyroxine
Dose should have been increased slowly upwards in 25mcg steps until on full replacement dose (typically 1.6mcg Levo per kilo of your weight per day) ….how much approximately do you weigh
guidelines on dose levothyroxine by weight
Even if we frequently start on only 50mcg, most people need to increase levothyroxine dose slowly upwards in 25mcg steps (retesting 6-8 weeks after each increase) until eventually on, or near full replacement dose
NICE guidelines on full replacement dose
nice.org.uk/guidance/ng145/...
1.3.6
Consider starting levothyroxine at a dosage of 1.6 micrograms per kilogram of body weight per day (rounded to the nearest 25 micrograms) for adults under 65 with primary hypothyroidism and no history of cardiovascular disease.
Also here
cks.nice.org.uk/topics/hypo...
pathlabs.rlbuht.nhs.uk/tft_...
Guiding Treatment with Thyroxine:
In the majority of patients 50-100 μg thyroxine can be used as the starting dose. Alterations in dose are achieved by using 25-50 μg increments and adequacy of the new dose can be confirmed by repeat measurement of TSH after 2-3 months.
The majority of patients will be clinically euthyroid with a ‘normal’ TSH and having thyroxine replacement in the range 75-150 μg/day (1.6ug/Kg on average).
The recommended approach is to titrate thyroxine therapy against the TSH concentration whilst assessing clinical well-being. The target is a serum TSH within the reference range.
……The primary target of thyroxine replacement therapy is to make the patient feel well and to achieve a serum TSH that is within the reference range. The corresponding FT4 will be within or slightly above its reference range.
The minimum period to achieve stable concentrations after a change in dose of thyroxine is two months and thyroid function tests should not normally be requested before this period has elapsed.