Hello dear people,
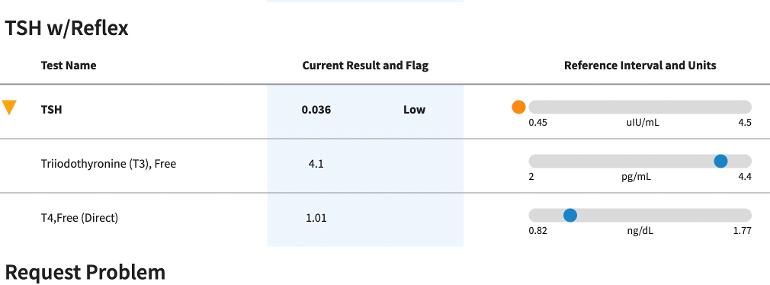
Here’s the short version: I’m having chest pain with a suppressed TSH, so I think the doctors will want to lower my meds when I’m actually feeling more hypo than hyper. Does anyone have any advice? I so appreciate the people here! The picture above is my last thyroid bloodwork from over a year ago.
Here’s the long version:
I’ve had my own Hashimotos under control for 15+ years with Armour thyroid. I’ve talked my primary care doctor into prescribing Armour, allowing me to adjust slightly when symptoms shift slightly, as long as the T4 and T3 bloodwork is within range. The doctor would prefer I be under the care of an endocrinologist, most of whom object to using natural thyroid, and also do not allow such a suppressed TSH. My TSH is always under 0.1, usually like 0.03 or somewhere near there.
But now I have chest pain that landed me in the ER, and the problem is that they are going to want the TSH to increase, even while I’m still having some hypothyroid symptoms.
At the ER, they did a 5-second EKG that seemed normal, but they did it while I was having no symptoms. The chest X-ray didn’t show anything, and the blood tests didn’t show the enzymes that indicate a heart attack. I’ve been doing ECG measurements on my Apple watch at least 10 times a day when I have chest pain, and they all come back normal sinus rhythm.
When I go in to have this looked at again, since the chest pain has continued, their reaction will be to lower my meds, but the thyroid-type symptoms I’m having point more toward hypothyroid rather than hyperthyroid:
Symptoms and stats: my resting heart rate is 59
I’m needing naps, which is usually my first indicator I need to increase thyroid meds slightly.
I’m having hair loss that the hairdresser noticed.
I’m gaining weight, but not drastically. But certainly not losing weight.
Blood pressure is always ideal, like 128/72 or something in that neighborhood.
If I had to guess where I’m at, I’d say that I should increase my thyroid meds slightly for a few weeks and see how it feels–but I’m worried that when I go in and get tested, as I’ll have to do with this level of chest pain, they will lower the meds and I will be miserable.
I even considered getting a private blood test so that I could know before I go in and deal with the doctors.
I was really sick for a month about a month ago, so I was wondering if the chest pain could be some kind of pericarditis from that. . . but the ER said that would normally show up on the chest x-ray.
I’ve been reading through all the past posts on the forum about “cardiac” and “TSH.” Thanks in advance for any thoughts!
Thanks,
Lost